

Spondylolisthesis is a forward slippage of one vertebral body over the one below. There are a variety of causes and classification schemes, but most can be described as either degenerative, caused by chronic inter-segmental instability involving degenerative disc and facet joints or isthmic, caused by developmental defects involving the posterior arch of the vertebra. Degenerative spondylolisthesis usually affects older patients, more frequently involves women at the L4/L5 vertebra level, and has relatively small slips (<30%) with associated stenosis. In contrast, isthmic spondylolisthesis usually affects patients younger than 50 years, primarily involves the L5 vertebra level, and may have quite severe progression (>50-100% slip) and associated structural abnormalities, including kyphosis.
The prevalence of spondylolisthesis ranges from 6% to 9% of the population, depending on the etiology studied and screening tools employed.1,2 Spondylolisthesis has not been reported in utero, in non-ambulatory patients, or mammals other than humans, implicating weight bearing forces unique to the upright bipedal spine. Spondylolisthesis and spondylolysis (a defect in the posterior arch without slip or translation) are seen in 4% of children at 6 years of age, 6% at maturity, and as many as 47% of athletes in high-risk sports such as gymnastics.1,2,3 Back pain is the most common complaint, but neurologic involvement may be seen with associated stenosis or progression and deformity. Children diagnosed prior to skeletal maturity or with slips greater than 50% are most likely to progress.4
Many patients with spondylolisthesis have no symptoms, and most likely do not require any significant treatment or intervention. Symptomatic patients are most frequently treated nonsurgically with NSAIDs, activity modification, physical therapy, and possibly epidural steroid injections. Bracing may be appropriate in some patients, particularly children with acute lesions.1,2 Surgical treatment is indicated when patients have significant disabling pain despite 6 months of adequate nonsurgical care or, less commonly, a progressive lesion. Treatment typically involves a posterior lumbar fusion. Instrumentation is thought to improve the fusion rate and clinical outcome,3 and decompression is included for patients with stenosis and associated radicular leg symptoms. Reduction of slips of greater than 50% remains controversial, but is thought to correct kyphosis and global sagittal balance, decrease the length of fusion, and protect against adjacent segment degeneration.4,5
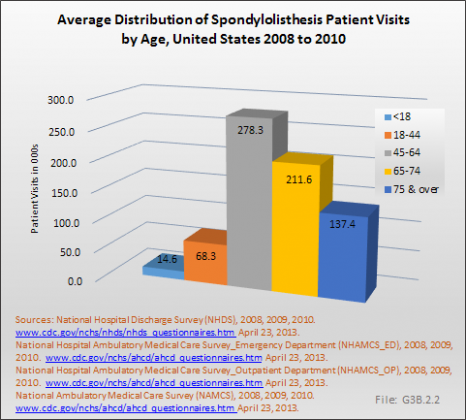
Analysis of various inpatient and outpatient databases from 2008–2011 showed 778,700 visits with a diagnosis for spondylolisthesis. The majority of these visits (81%) were outpatient visits, primarily to a physician office. More than two in three (69%) visits for spondylolisthesis were by females with an average age between the late 50s or early 60s. More recent data from 2010–2011 demonstrate 185,400 hospital or emergency department discharges for spondylolisthesis with similar age and sex distribution (Reference Table 3.1.1 PDF [1] CSV [2] and Table 3.1.2 PDF [3] CSV [4]).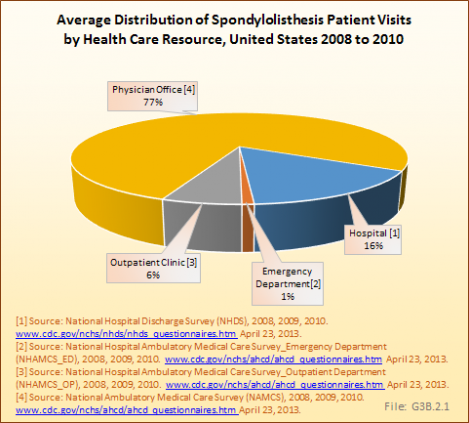
In 2011, there were 146,100 hospital discharges for spondylolisthesis reported in the HCUP NIS database. The average length of stay for these patients was 4 days, and tended to trend slightly upwards with age. The mean charges for hospital discharges with a diagnosis of spondylolisthesis was $93,900, which was unexpectedly higher than all other deformity codes evaluated and statistically similar to costs associated with hospital discharges for patients with complications of spine surgery diagnosis.
Among the much smaller sample of patients with a diagnosis of spondylolisthesis who were first seen in the emergency department (ED) and transferred to inpatient status, the average length of stay was slightly longer (5.2 days), but with lower average charges of $46,800. The proportion of patients with a spondylolisthesis diagnosis hospitalized after being seen in the ED who had a surgical procedure was much lower than those reported in the inpatient database. (Reference Table 3.4.1 PDF [5] CSV [6]; Table 3.4.2 PDF [7] CSV [8]; and Table 3.5.1 PDF [9] CSV [10]) 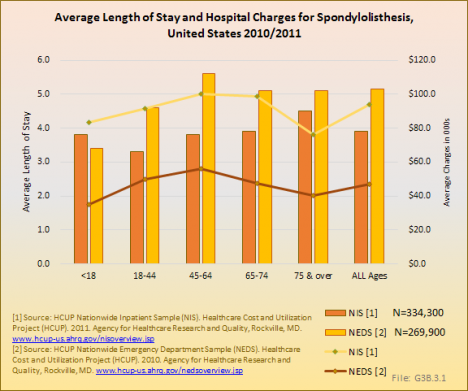
Nearly two-thirds (61%) of inpatients with a spondylolisthesis diagnosis were discharged from the hospital to home, although the proportion was lower when hospitalized after visiting the ED. Another 15% to 18% went home with home health care. One in five (21%) were transferred to a skilled nursing facility. Age is a major factor in discharge status, with 44% of patients age 75 years and older discharged to skill nursing/intermediate care. (Reference Table 3.3.1 PDF [11] CSV [12] and Table 3.3.2 PDF [13] CSV [14])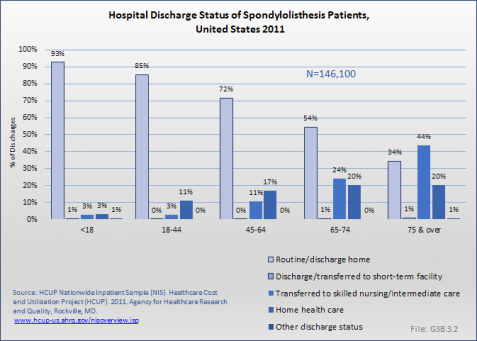
Three out of four patients (75%) hospitalized with a diagnosis of spondylolisthesis were treated with a spinal fusion. About one-half were treated with instrumentation and decompression. Patients with spondylolisthesis often received more than one procedure in their stay. The overall costs for treatment of spondylolisthesis would be much higher than simply the hospitalization cost. The direct cost of nonsurgical treatments, such as medications, therapy, injections, braces, etc., and the indirect costs associated with treatment of this condition such as lost wages, non-productive time away from work, costs of medical care providers, are not included in these databases although they may be quite substantial. (Reference Table 3.5.1 PDF [9] CSV [10])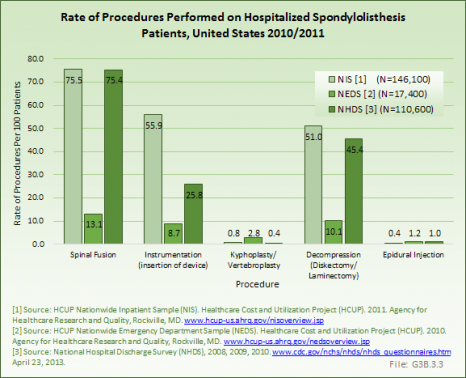
Links:
[1] https://bmus.latticegroup.com/docs/T3.1.1.pdf
[2] https://bmus.latticegroup.com/docs/T3.1.1.csv
[3] https://bmus.latticegroup.com/docs/T3.1.2.pdf
[4] https://bmus.latticegroup.com/docs/T3.1.2.csv
[5] http://bmus.latticegroup/docs/T3.4.1.pdf
[6] http://bmus.latticegroup/docs/T3.4.1.csv
[7] http://bmus.latticegroup/docs/T3.4.2.pdf
[8] http://bmus.latticegroup/docs/T3.4.2.csv
[9] http://bmus.latticegroup/docs/T3.5.1.pdf
[10] http://bmus.latticegroup/docs/T3.5.1.csv
[11] https://bmus.latticegroup.com/docs/T3.3.1.pdf
[12] https://bmus.latticegroup.com/docs/T3.3.1.csv
[13] https://bmus.latticegroup.com/docs/T3.3.2.pdf
[14] https://bmus.latticegroup.com/docs/T3.3.2.csv