

Osteoporosis was traditionally thought of as a condition affecting only women. Although approximately 80% of patients with the condition are female, it is being increasingly diagnosed among men. This increased incidence may reflect a greater awareness of the condition among men, rather than a true increase in incidence.
There are significant sex-based differences in osteoporosis. Osteoporosis in men tends to occur at an older age, unless another health condition intervenes. Osteoporosis in women is more likely primary and a result of estrogen loss, while osteoporosis in men is more likely to be secondary to another health condition, especially alcohol over-consumption, loss of testosterone, and use of corticosteroids.
Low impact, or fragility, fractures, frequently occurring as the result of a simple fall, are more common among women, reflecting the higher incidence of osteopenia or osteoporosis. In 2011, 71% of partial hip replacements, most commonly performed to treat hip fractures, were performed on women. (Reference Table 9A.4.2 PDF [1] CSV [2]) For both sexes, the initial fragility fracture is the most significant risk factor for additional fractures and represents an opportunity for secondary prevention. Unfortunately, the likelihood of evaluation and attempts at secondary prevention measures are low for both sexes. However, men, more than women, are even less likely to be evaluated and treated for osteoporosis after the initial fragility fracture.1
For both men and women, low-impact fractures related to poor bone health have significant impact on function, morbidity, and mortality. Vertebral fractures, the most common fracture related to low bone mass, can lead to chronic pain, reduced subjective health status, and limitation in activities. The incidence of vertebral fractures increases with age for both sexes, although this is more pronounced among women.2 After adjusting for age and bone mineral density, sex-based risk for sustaining a vertebral fracture tends to be no longer significant.1 Smoking, alcohol consumption, and physical activity are known to impact bone health. However, studies examining their association with the risk of vertebral fractures have provided inconclusive evidence of sex-based differences in degrees of impact.3 The rate of mortality also is increased among those sustaining a vertebral fracture. However, Hasserius et al noted that the pattern of differences in mortality differed by sex: increased mortality in women was noted during the first decade after the fracture, especially the first 5 years; the greatest divergence in mortality among men was most significant during the first 3 years after the fracture.4 This is similar to the data available for outcome after fragility fractures of the hip. Hip fractures also lead to increased rates of disability and mortality; however, mortality is substantially higher among men sustaining a hip fracture, especially during the first year after the fracture. These differences in mortality after low-impact fracture, especially in the first few years after fracture, may reflect the differences in etiology of osteoporosis. Men, as previously noted, are more likely to have secondary osteoporosis and be older at the time of fracture; both of these most likely contribute to increased rates of mortality.
Osteoporosis is often not the principal diagnosis code related to a health care visit, as the condition is usually an underlying cause of another condition, in particular, fragility fractures that often occur after a fall or other seemingly minor incident. Many times in such health care visits, osteoporosis may not even be listed as a condition. Still, in 2011, primary osteoporosis was listed in 2.3 million hospital discharges and emergency department visits as a reason for the visit. Fragility fractures occurred in 4.0 million visits. For 395,500 visits or discharges for fragility fractures, or 10%, primary osteoporosis was also listed as a condition for the visit. The highest proportion of fractures to the vertebrae and stress fractures were diagnosed in women.
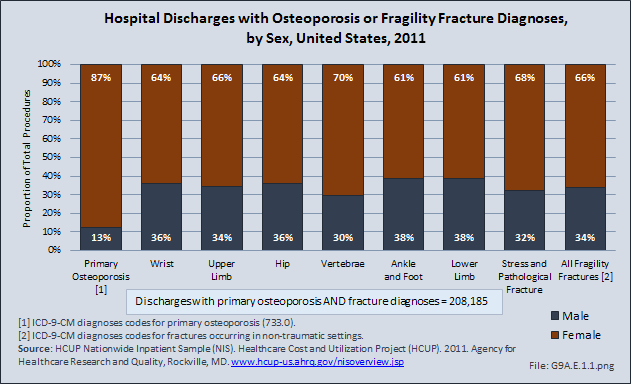
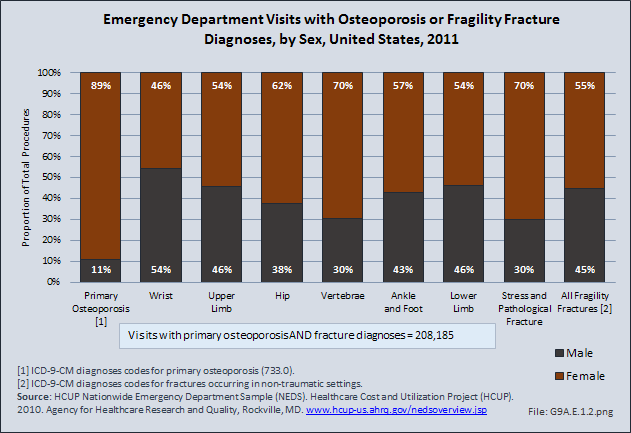
Two-thirds of hospital discharges for fragility fractures occurred in women, while 87% of primary osteoporosis diagnoses were in women. Primary osteoporosis was found in a similar proportion of emergency department visits (89%) for women; however, fragility fractures were split 45% males to 55% females.
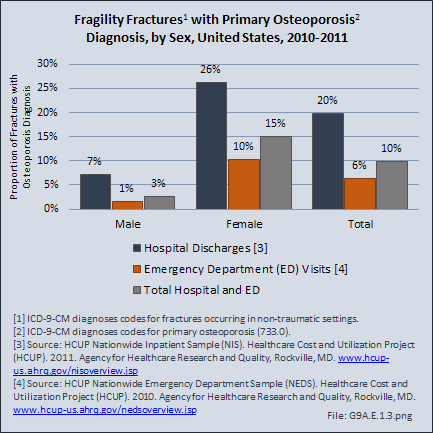
Women also were more likely to have a primary osteoporosis diagnosis with a fragility fracture, accounting for 26% of hospital discharges and 10% of emergency department visits. Among men, both diagnoses were found in 7% of hospital discharges and only 1% of emergency department visits. The noted incidence of osteoporosis among men in this situation is most likely underreported as, noted above, men are less likely than women to be evaluated for osteoporosis, even after sustaining a low impact fracture. Evaluation of bone health in men and women after sustaining a low impact fracture and initiation of secondary fracture prevention measures are areas that require significant attention and improvement. (Reference Table 9A.5 PDF [3] CSV [4])
Links:
[1] https://bmus.latticegroup.com/docs/T9A.4.2.pdf
[2] https://bmus.latticegroup.com/docs/T9A.4.2.csv
[3] https://bmus.latticegroup.com/docs/T9A.5.pdf
[4] https://bmus.latticegroup.com/docs/T9A.5.csv