

Osteoporosis-related fractures are associated with a substantial increase in the utilization of health services for both acute and long-term care. Fracture risk increases with age,1,2 as does the burden of disease in terms of morbidity, mortality, and costs.3 Here we focus on the effects of osteoporosis and related fractures on health care utilization.
While the incidence of hip fracture appears to have declined overall since the mid 1990s, as discussed in a previous section [1], hospital discharges from the MEPS database related to osteoporosis were 44% greater in 2009 to 2011 than they were in the years from 1996 to 1998. Recent years, however, have shown a decline after peaking in 2001 to 2003. (Reference Table 10.2 PDF [2] CSV [3]) This increase in hospitalizations likely reflects the increase in older population cohorts as the Boomer generation enters the prime years for fracture incidence.
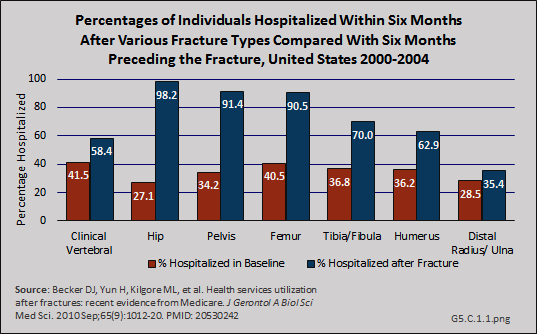
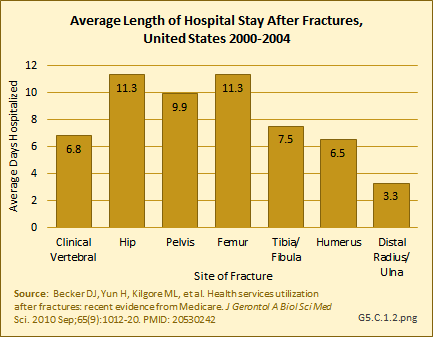
In a study among Medicare beneficiaries, the 65 years and older population, experiencing hip fractures in the years 2000 to 2004, 98.2% were hospitalized in the six months following the fracture compared to 27.1% hospitalized at least once in the prior six months for other reasons.1 Thus, hip fractures were associated with a 71% increase in the probability of being hospitalized. The average length of stay for hip and upper leg (femur) fractures was more than 11 days. (Reference Tables 5.3 PDF [4] CSV [5] and 5.4 PDF [6] CSV [7])
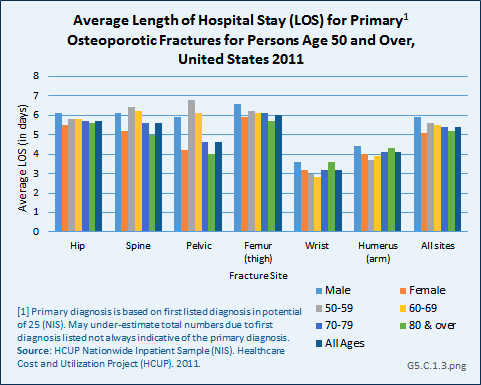
Using recent 2011 data from the NIS hospital discharge database, an average hospital stay of 5.5 days was reported for people age 50 years and older with a primary (first) diagnosis of fragility fracture. While it might be assumed the inclusion of younger-age patients could account for this difference from the earlier study, age was not a factor in length of stay. Sex was a more significant factor, with males staying nearly a day longer than females. With the exception of wrist and arm fractures, site of the fracture was also not a factor. (Reference Table 5.5 PDF [8] CSV [9])
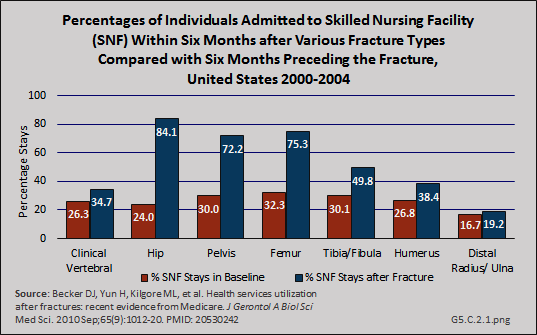
Patterns similar to hospitalization for the Medicare population were reported for use of skilled nursing facility and home health services following hospitalization before and after fractures, although the rates for these services were somewhat lower. Hip fractures were associated with an 84% increase in probability of a stay in a skilled nursing facility.1 (Reference Tables 5.3 PDF [4] CSV [5] and 5.4 PDF [6] CSV [7])
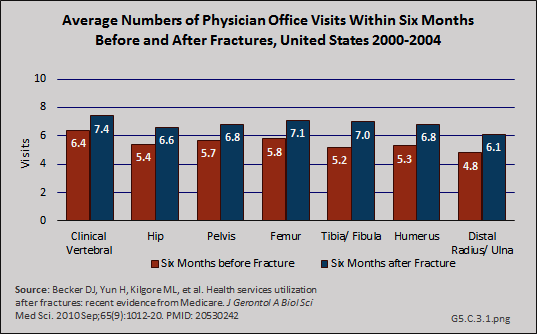
In a recent study, the effect of fracture on physician office visits using a baseline of visits six months before fracture and comparing it to six months after fracture, was less than for hospitalization, but still substantial.1 Fractures of the tibia/fibula had the greatest increase in physician office visits (35% increase in probability of a visit), but this could be because of higher rates of transfer to nursing home care for hip, pelvis, and femur fractures shown in studies discussed previously. (Reference Table 5.6 PDF [10] CSV [11])
Following fractures, utilization of physical and occupational therapy services increased by similar proportions.1
Although the mean number of ambulatory physician visits for osteoporosis care from the MEPS study, the data upon which estimated cost burden from osteoporosis [12] is based, declined between 1996 and 1998 and between 2009 and 2011, the total number of visits over this timeframe increased by 67% because of the larger number of people with osteoporosis. Because the MEPS data is based on only an osteoporosis diagnosis rather than a fracture diagnosis, the actual numbers may be larger than reported.
Again, using the MEPS, the mean number of home health visits for osteoporosis between 1996 and 1998 was 7.7; from 2009 to 2011 it was 7.4. However, the total number of visits rose from 24.3 million to 47.5 million due to the rise in reported prevalence of osteoporosis. Ambulatory nonphysician health care visits nearly tripled, increasing from 10.7 million to 28.9 million, due to an increase in both mean number of visits and the share of persons with reported osteoporosis who made at least one such visit. (Reference Table 10.2 PDF [2] CSV [3])
Serious adverse outcomes following hip fractures include mortality, debility requiring institutional care, and destitution (poverty) sufficient to qualify for Medicaid enrollment. In a recent study of Medicare beneficiaries, the population age 65 years and older, individuals experiencing hip fracture had more than double the risk of death, an almost four-fold increased risk of becoming a nursing home resident, and more than double the risk of enrolling in Medicaid within one year of the fracture.1 (Reference Table 5.7 PDF [13] CSV [14])
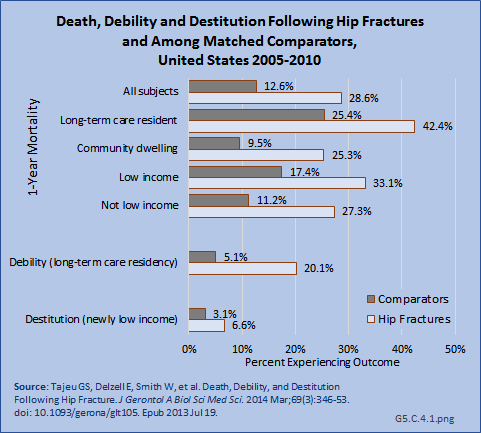
Two recent studies of the Medicare population support a significant decline in mortality from hip fractures in recent years, with reported mortality rates of 22%2 and 30%3 in the first year following fracture. However, hip fracture remains a major mortality risk 2- to 8-fold higher than non-hip-fracture matched controls.3
Links:
[1] http://www.boneandjointburden.org/2014-report/vb3/hip-fracture-trends
[2] https://bmus.latticegroup.com/docs/T10003.2.pdf
[3] https://bmus.latticegroup.com/docs/T10003.2.csv
[4] https://bmus.latticegroup.com/docs/T5.3.pdf
[5] https://bmus.latticegroup.com/docs/T5.3.csv
[6] https://bmus.latticegroup.com/docs/T5.4.pdf
[7] https://bmus.latticegroup.com/docs/T5.4.csv
[8] https://bmus.latticegroup.com/docs/T5.5.pdf
[9] https://bmus.latticegroup.com/docs/T5.5.csv
[10] https://bmus.latticegroup.com/docs/T5.6.pdf
[11] https://bmus.latticegroup.com/docs/T5.6.csv
[12] http://www.boneandjointburden.org/2014-report/x0/economic-cost
[13] https://bmus.latticegroup.com/docs/T5.7.pdf
[14] https://bmus.latticegroup.com/docs/T5.7.csv