 [7]
[7] 

Previous sections in this text clearly demonstrate the large percentage of healthcare visits that are attributable to musculoskeletal conditions. Most of the data used to establish these estimates concern adult patients. Unfortunately, there is significantly less information regarding the burden of these conditions in young patients.
Studies, however, do support that pediatric musculoskeletal conditions similarly account for a significant portion of visits to medical providers. For instance, de Inocencio reported that greater than 6% of total visits to pediatric clinics were for musculoskeletal pain.1 Schwend reported that approximately one third of pediatric medical problems are related to the musculoskeletal system.2 In a population-based study in Ontario, Canada, Gunz reported that 1 in 10 children made a healthcare visit for a musculoskeletal problem and that 13.5% of all visits for musculoskeletal disease were made by patient’s age 0 to 19 years.3 Four in 1,000 children are reported by parents as having difficulty with activities of daily living due to musculoskeletal conditions. A search of the National Health Interview Survey [1] (NHIS) child sample revealed that musculoskeletal conditions accounted for 1.6% of parent-reported health conditions in 73.5 million healthcare visits for children and adolescents age 0 to 17 years in the US from 2013 to 2015. This proportion was greatest at 2.4% in the 14- to 17-year-old age group. (Reference Table 7C.0 PDF [2] CSV [3])
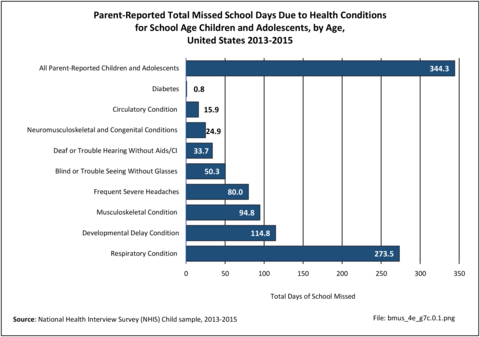
The evaluation and treatment of these pediatric musculoskeletal conditions resulted in approximately 94.8 million missed school days per year from 2013 to 2015, accounting for 27.5% of all missed school days. Musculoskeletal conditions are surpassed only by respiratory infections and developmental delay as a cause of missed school days. Children aged 5 to 9 years old missed the highest number of school days due to musculoskeletal pain. (Reference Table 7C.0.1 PDF [4] CSV [5])
Children with musculoskeletal conditions also commonly have other medical problems. According to the National Health Interview Survey from 2013 to 2015, these are most commonly respiratory conditions followed by developmental delay. Of children with musculoskeletal conditions, 48% also have a diagnosed respiratory condition and 36% have developmental delay. (Reference Table 7C.0.2 PDF [8] CSV [9])
Despite the significant contribution made by musculoskeletal conditions in the total US healthcare burden, research for pediatric musculoskeletal conditions is grossly underfunded. Of the $3.25 billion in National Institutes of Health (NIH) research funding for all pediatric conditions in 2013, only $46.8 million, or 1.4% of total pediatric medical research funding, went toward pediatric musculoskeletal research. Even under the umbrella of funding specifically for musculoskeletal research, pediatric-specific research is under-represented. Of the $424.4 million in funding for the National Institute of Arthritis and Musculoskeletal and Skin Disease (NIAMS) in 2013, this same $46.8 million represented only 11% of total musculoskeletal research dollars.4
In order to perform a comprehensive review of the burden of musculoskeletal disease in children and adolescents, all conditions that are direct musculoskeletal diagnoses or have musculoskeletal implications were considered for this section. This chapter was divided into separate clinically relevant sections to better understand the burden of each. These sections include musculoskeletal infections, deformity, trauma, neuromuscular conditions, syndromes with musculoskeletal implications, sports injuries, neoplasms, skeletal dysplasias, rheumatologic conditions, medical problems with musculoskeletal implications, and pain syndromes.
Healthcare visits and hospitalization data are derived from diagnostic codes for each of the conditions presented. These codes are available in the ICD-9-CM Codes [12] section of this topic. Total healthcare visits are the sum of cases seen in physicians’ offices (National Ambulatory Medical Care Survey), outpatient clinics (National Hospital Ambulatory Medical Care Survey), emergency departments (Nationwide Emergency Department Sample), and hospital discharges (Nationwide Inpatient Sample). The largest database used is the Healthcare Cost and Utilization Project [13] (HCUP) Nationwide Emergency Department Sample (NEDS), which estimates approximately 32.5 million weighted visits of children and adolescents through the age of 20 years. These four databases were analyzed for the ages 0 through 20 years, with subsets of data by age groups under 1 year, ages 1 to 4 years, 5 to 9 years, 10 to 13 years, 14 to 17 years, and 18 to 20 years.
Each database includes multiple variables to define diagnoses, ranging from three possible diagnoses in the physicians’ office and outpatient clinic data sets to 25 possible diagnoses in the HCUP National Inpatient Sample (NIS) database. If a diagnosis code is listed in any of the possible diagnosis variables, the record is coded as presenting with that condition. If the diagnosis code is listed in the first diagnosis variable, it is coded as the primary diagnosis. However, the databases do not permit diagnostic verification. The first diagnosis listed may not be the primary reason for the visit, but a contributing cause. Further, there is the potential for overlap in diagnosis of related conditions. It is also possible diagnoses codes used for reimbursement purposes may be inaccurate. Therefore, these numbers provide only a guide to the impact of major childhood musculoskeletal conditions.
Injuries include two categories: sports injuries and injuries due to a traumatic event. Sports injuries are identified by type of sports activity using the United States Consumer Product Safety Commission’s National Electronic Injury Surveillance System [16] (NEISS), with annual injuries averaged across the years of 2014 to 2016. Because sports injuries cases are not analyzed by ICD-9-CM codes, they may duplicate trauma injury cases cited from the previously discussed databases.
The 11 categories of musculoskeletal conditions that follow represent the most common healthcare reasons for which children and adolescents are seen in doctors' offices, emergency departments, and hospitals. Many of these conditions, such as the skeletal dysplasias, are relatively rare, diagnosed infrequently in the healthcare system, and have little data available on prevalence and burden. Though rare, they may result in significant morbidity and often require lifelong medical interventions and, therefore, warrant discussion.
In 2013, more than 18 million children and adolescents age 20 years and younger received treatment in medical centers, physicians’ office, and hospitals for a condition that included a musculoskeletal-related condition. More than 65% were for the treatment of traumatic injuries. The second most common diagnosis is a pain syndrome, accounting for more than 1 in 10 visits (15%). Pain syndromes include amplified musculoskeletal pain and benign limb pains, along with less common juvenile primary fibromyalgia syndrome, reflex sympathetic dystrophy, and benign hypermobility syndrome. The third most frequent diagnosis is sports injuries, accounting for just over 10% of all visits. The discussion of sports injuries utilizes a unique database that is not based on ICD-9-CM codes; it is likely there is overlap between traumatic injuries and sports injuries. (Reference Table 7C.1.1 PDF [18] CSV [19])
More than two-thirds (70%) of visits by children and adolescents for a condition that included a musculoskeletal-related condition were to physicians’ offices or outpatient clinics. Hospital discharges accounted for less than 3% of total visits. Healthcare visits that included a musculoskeletal-related condition represented 7% of visits made by children and adolescents for any reason but were more than 15% of all visits to the emergency department. (Reference Table 7C.1.1 PDF [18] CSV [19])
Among the 246 million healthcare visits by children and adolescents in 2013, 14.4 million had a primary diagnosis of a musculoskeletal-related condition. The greater proportion (64%) were for the treatment of traumatic injuries, with the second and third most common primary diagnoses being sports injuries (13%) and pain syndrome (12%). Although all other musculoskeletal-related conditions accounted for 13% of total healthcare visits for a musculoskeletal-related condition, they nevertheless remain serious health concerns for children and adolescents. (Reference Table 7C.1.2 PDF [24] CSV [25])
Again, many visits were to physicians’ offices and outpatient clinics (70%), while visits to an emergency department with a primary musculoskeletal-related condition diagnosis accounted for 29% of visits. Hospital discharges accounted for less than 1% of total visits with a primary musculoskeletal diagnosis. Healthcare visits that included a primary diagnosis of a musculoskeletal-related condition represented 6% of visits made by children and adolescents for any reason but were 13% of all visits to the emergency department. (Reference Table 7C.1.2 PDF [24] CSV [25])
Musculoskeletal infections included in this section are osteomyelitis, septic arthritis, soft tissue infections (myositis), Lyme disease, and tuberculosis. Osteomyelitis and septic arthritis are the most common form of pediatric musculoskeletal infections, and most often occur in the first decade of life in previously healthy children. Infectious myositis refers to conditions causing inflammation in muscles and may be part of a systemic (whole body) infection, especially a viral infection. Lyme disease is caused by a bite from a deer tick and is less common than osteomyelitis and septic arthritis. It is more prevalent in the Northeastern and Midwestern regions of the United States.1 Tuberculosis (TB) has become much less common in the United States over the last few decades but has increased in incidence in developing countries secondary to immunodeficiency and multidrug resistance. TB infections involve the musculoskeletal system in 2% to 5% of cases.2
Community-acquired Staphylococcus aureus (CA-SA) is the most common infecting organism in pediatric musculoskeletal infections and is typically treated with a first-generation cephalosporin, such as cefazolin. Over the past decade, methicillin-resistant Staphylococcus aureus (MRSA) has become prevalent and requires treatment with second-line antibiotics such as clindamycin or vancomycin.3 As MRSA infections have become more prevalent, the disease course for patients with these infections have become much more severe, with greater systemic disease requiring multimodal and multidisciplinary treatments including medical, surgical, and critical care. Patients are often hospitalized for extended periods and most require continued care with long-term antibiotic treatment after discharge. Multiple surgical debridements are often required. Complications of musculoskeletal infections include growth deformity, fractures, and arthritis, and may result in long-term morbidity and dysfunction.
Musculoskeletal infections were diagnosed in 61,400 children and adolescent healthcare visits in 2013, of which 41,800 had a primary diagnosis of musculoskeletal infection. Of this total, 14,000 children and adolescents were hospital discharges, with 8,300 hospitalizations for a primary diagnosis of a musculoskeletal infection. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Males were more likely to be hospitalized with a musculoskeletal infection than females. The most common age group was between 5 and 9 years old. Musculoskeletal infections as a primary diagnosis accounted for 1.6% of hospital discharges for any musculoskeletal-related condition, but only 0.1% of hospital discharges for all healthcare reasons for children and adolescents age 20 years and younger. (Reference Table 7C.2 PDF [30] CSV [31])
Total charges averaged $76,900 for a mean 8.5-day stay when children and adolescents were hospitalized with a diagnosis of musculoskeletal infection along with other medical conditions. With a primary diagnosis of infection, the stay was shorter (5.9 days), and mean charges were less at $48,300. Total hospital charges for all primary musculoskeletal infection discharges in 2013 were $400.9 million. (Reference Table 7C.2 PDF [30] CSV [31])
Deformity in children and adolescents is subdivided into five sections: upper extremity, lower extremity, hip and pelvis, spine, and other/unspecified.
Upper extremity deformity includes diagnoses such as polydactyly, syndactyly, and reduction deformities such as amyelia and longitudinal deficiencies of the upper extremity, and other congenital deformities such as synostosis, Madelung deformity, and Apert syndrome. A complete listing of deformity codes can be found in the ICD-9-CM Child and Adolescents Codes [12].
Lower extremity deformity includes diagnoses such as polydactyly, syndactyly, and reduction deformities such as amyelia and longitudinal deficiencies of the lower extremity, genu varum, genu valgum, and other congenital developmental deformities such as clubfoot and flatfoot.
Hip and pelvis deformity include diagnoses such as coxa valga, coxa vara, slipped capital femoral epiphysis, pelvic deformity, Legg Calves Perthes disease, and developmental dysplasia of the hip. Hip deformity is among the most common developmental deformities in childhood. Developmental dysplasia of the hip is estimated to occur in between 1 in 100 to 1 in 1000 newborns.1
Spine deformity includes anomalies of the spinal cord such as syringomyelia and diastomatomyelia, as well as deformities of the vertebral column such as scoliosis, kyphosis, spondylolysis, spondylolisthesis, and congenital spinal anomalies.
Other and unspecified deformities include deformities of the chest wall such as pectus excavatum and pectus carinatum, as well as nonspecific deformity diagnoses.
Deformity of the spine represented the largest share of hospitalizations (40.7%) in 2013, followed by the lower extremity at 29% and upper extremity at 19.1%. (Reference Table 7C.3 PDF [36] CSV [37])
Musculoskeletal deformities were diagnosed in 1.7 million children and adolescent healthcare visits in 2013, of which 958,900 had a primary diagnosis of musculoskeletal deformity. Among the total with any diagnoses of deformity, 108,100 children and adolescents were hospital discharges, with 27,500 hospitalizations for a primary diagnosis of a musculoskeletal deformity. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Females had a slightly higher rate of overall deformity diagnoses with hospitalization, accounting for 52% of primary diagnosis. Neonates had a high rate of musculoskeletal deformity for any diagnosis with hospitalization (24.4%) but accounted for only 0.1% of primary hospitalizations of all musculoskeletal diagnoses. Primary diagnosis of musculoskeletal deformity with hospitalization was highest between the ages of 10 and 17 years.
Musculoskeletal deformity as a primary diagnosis accounted for 5.5% of hospitalizations for any musculoskeletal condition diagnosis, but only 0.4% of hospitalizations for any healthcare reason for children and adolescents age 20 years and under. (Reference Table 7C.3 PDF [36] CSV [37])
Total charges averaged $70,700 for a mean 6.3-day stay when children and adolescents were hospitalized with a diagnosis of musculoskeletal deformity along with other medical conditions. With a primary diagnosis of deformity, the stay was shorter (4.1 days), but mean charges were much higher at $100,200, primarily due to the higher charges for children and adolescents age 10 years and older. Total hospital charges for all primary musculoskeletal deformity discharges in 2013 were $2.76 billion. (Reference Table 7C.3 PDF [36] CSV [37])
Traumatic injury is the leading cause of death in children and adolescents, accounting for 20,000 deaths per year in the United States.1 Although most musculoskeletal injuries are not life threatening, they do account for approximately 10% to 25% of injuries in this age group.2
The pediatric musculoskeletal system is different from that of an adult, and, therefore, the assessment, treatment, and outcome of injuries is different. Pediatric bone is more elastic, and with a capacity for growth, there exists superior remodeling capability. Because of this, many fractures that require surgical treatment in adults may be treated nonoperatively in children. On the other hand, injury to the growing child can result in growth deformity that can lead to long-term morbidity and the need for reconstructive treatments. This section subdivides pediatric musculoskeletal trauma into six sections: upper extremity, lower extremity, hip and pelvis, spine and trunk, birth trauma, and nonaccidental trauma (child abuse). (Reference Table 7C.4 PDF [45] CSV [46])
Trauma resulting in musculoskeletal injury was diagnosed in 11.8 million children and adolescent healthcare visits in 2013, of which 79% (9.3 million) had a primary diagnosis of musculoskeletal injury. Only a small number were serious enough to require hospitalization. Among any trauma musculoskeletal injury diagnoses, 215,200 children and adolescents were hospitalized, with 65,600 having a primary diagnosis of a musculoskeletal injury. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Males had higher injury rates with hospitalization than females for both any diagnoses (60% of injuries) and as a primary diagnosis (67% of injuries). Hospitalization for musculoskeletal injuries were highest among adolescents age 14 years and older. Neonates under the age of one year had a high rate of musculoskeletal injury for any diagnosis with hospitalization, primarily due to a diagnosis of birth trauma (99%), but a much lower rate of hospitalization with a primary trauma diagnosis (0.5% of musculoskeletal diagnoses in this age bracket).
Musculoskeletal injury as a primary diagnosis accounted for 13% of hospitalizations for any musculoskeletal condition diagnosis, and 1.0% of hospitalizations for any healthcare reasons for children and adolescents age 20 years and younger. For all but the youngest age, which is skewed by birth trauma, primary diagnosis of trauma accounted for 13.5% to 21.9% of all hospitalization for any musculoskeletal diagnoses. (Reference Table 7C.4 PDF [45] CSV [46])
Trauma to the upper extremity account for half (50%) of all trauma healthcare visits by children and adolescents. This was followed by lower extremity trauma (38%). Spine and trunk injuries were 8%, with hip and pelvis injuries at 2%. A diagnosis of birth trauma was less than 1% of all healthcare visits but accounted for more than half (53%) of hospital discharges for musculoskeletal trauma diagnoses. Child abuse was reported in 1% of all healthcare visits for trauma. (Reference Table 7C.1.1 PDF [18] CSV [19])
Total charges averaged $37,100 for a mean 4.2-day stay when children and adolescents were hospitalized with a diagnosis of musculoskeletal injury along with other medical conditions. With a primary diagnosis of musculoskeletal injury, the stay was shorter (3.1 days), but mean charges were higher at $46,300, likely due to the high number of birth trauma cases. Mean charges were highest for older adolescents (18 to 20 years) followed by neonates. Total hospital charges for all primary musculoskeletal injury discharges in 2013 were $3.04 billion. (Reference Table 7C.4 PDF [45] CSV [46])
Common pediatric neuromuscular conditions include cerebral palsy, myelomeningocele (spina bifida), muscular dystrophy, spinal muscular atrophy, hereditary motor sensory neuropathies, Friedrich ataxia, and Rett syndrome. This is a heterogeneous group of disorders with varying degrees of severity and involvement. Although some children and adolescents with these diagnoses can lead a relatively normal life and participate in normal activities, many are completely dependent on their care provider. Most patients lie somewhere between the two ends of this range and require varying amounts of care for their condition. The overall burden of these diagnoses is not limited to number of visits or admissions. These diagnoses also carry significant indirect costs including, but certainly not limited to, lost wages by the caregiver who is unable to go to work; out-of-pocket costs for necessities such as therapy, bracing, and wheelchairs; and the significant emotional impact on the family and care provider.
Neuromuscular conditions were diagnosed in 554,500 children and adolescent healthcare visits in 2013, of which 214,600 had a primary diagnosis of a neuromuscular condition. About 1 in 10 (11%) children and adolescents with any neuromuscular diagnoses were hospitalized (61,200), but fewer than 2% (4,100) with a primary neuromuscular diagnosis had a hospital discharge. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Males were slightly more likely to be hospitalized than females for both any neuromuscular diagnoses and as a primary diagnosis. Children ages 6 to 10 years had the highest rate of hospitalization, both with any diagnoses and as a primary diagnosis. Rates of hospitalization declined past 9 years old.
Neuromuscular conditions as a primary diagnosis accounted for 0.8% of hospitalizations for any musculoskeletal condition diagnosis and only 0.1% of all hospitalizations for any healthcare condition. (Reference Table 7C.5 PDF [55] CSV [56])
Cerebral palsy was diagnosed in two-thirds (65%) of hospital discharges. Spina bifida and muscular dystrophy represented 18% and 7% of discharges, respectively.
Total charges averaged $75,700 for a mean 6.7-day stay when children and adolescents were hospitalized with a diagnosis of a neuromuscular condition along with other medical conditions. With a primary neuromuscular diagnosis, the stay was longer (7.2 days), and mean charges were higher at $92,000. Mean charges and length of stay were highest for the youngest patients, neonates. Total hospital charges for all primary neuromuscular discharges in 2013 were $377.2 million. (Reference Table 7C.5 PDF [55] CSV [56])
Syndromes with musculoskeletal implications include those diagnoses that may result in or be associated with musculoskeletal problems or deformities. The most common syndromes with musculoskeletal implications include Marfan syndrome, Ehlers Danlos syndrome, Down syndrome, and neurofibromatosis. These patients may have musculoskeletal problems including scoliosis, pectus deformities, hip dysplasia, and flatfeet. Patients with neurofibromatosis may have congenital pseudarthrosis of the tibia. Many of these patients will require treatment for these musculoskeletal problems. Treatment, however, must be tailored to each individual patient as these syndromes often affect multiple body systems and require involvement of multiple medical disciplines.
Syndromes with musculoskeletal implications were diagnosed in 383,200 children and adolescent healthcare visits in 2013, of which 126,300 had a primary diagnosis of one of these conditions. About 1 in 10 (9%) children and adolescents with any syndrome with musculoskeletal implications diagnoses were hospitalized (29,800), but less than 1.2% (600) with a primary diagnosis of a syndrome with musculoskeletal implications had a hospital discharge. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Male were more likely than females to have a hospital discharge with any syndrome with musculoskeletal implications diagnoses as well as a primary diagnosis. Infants and young children under the age of 5 years had the highest rate of hospitalization for any diagnoses of syndromes with musculoskeletal implications. The number of hospitalizations with a primary diagnosis was too small for analysis by age.
Any diagnoses of syndromes with musculoskeletal implications accounted for 5.4% of hospitalizations for any musculoskeletal condition diagnosis, and 0.4% of all hospitalizations for any healthcare condition. Hospitalizations with a primary diagnosis were 0.1% of all musculoskeletal diagnoses. (Reference Table 7C.6 PDF [63] CSV [64])
Total charges averaged $78,500 for a mean 7.9-day stay when children and adolescents were hospitalized with a diagnosis of a syndrome with musculoskeletal implications condition along with other medical conditions. The number of hospitalizations with a primary diagnosis of a syndrome with musculoskeletal implications was too small for analysis of hospital charges. (Reference Table 7C.6 PDF [63] CSV [64])
Athletic participation by children and adolescents increased dramatically between 1997 and 2008,1 with participation declining slightly since the 2008 peak.2 Over the past several years, participation in some sporting activity has slowly increased with 69% of children playing a sport at least one day during the year in 2017. However, team sports participation regularly continues to slowly decline with only 37% of children consistently participating in a team sport.3
Since the late 1990s, athletic specialization has increased, resulting in earlier focus on single sports. As a result, there has been a commensurate increase in pediatric sports-related injuries, both acute and related to chronic overuse.4 Pediatric and adolescent athletes are anatomically and physiologically different from adult athletes, and therefore are at risk to sustain different injuries. Coordination and mechanics are less developed in pediatric athletes, placing them at greater risk for injuries related to falls and collisions. Growing athletes are at risk for most of the same injuries as adult athletes but are uniquely susceptible to injuries about the physeal (growth plates in bones that undergo endochondral ossification) and growth cartilage. Not only do these physeal and apophyseal injuries5 require unique treatments, but they may also result in growth derangement that can lead to deformity and have long-term consequences. Adolescent female athletes also have been shown to have a two- to nine-fold greater risk of knee injuries, which may be related to age and gender-specific differences in anatomy, neuromuscular control, and hormone levels.6 Common pediatric sports-related injuries include anterior cruciate ligament (ACL) and meniscal tears, tibial eminence fractures, osteochondritis desiccans lesions, patellofemoral instability, Osgood Schlatter syndrome, little league shoulder and elbow, pelvic avulsion fractures, and distal radius epiphysitis.
On average across the years from 2014 to 2016, 1.6 million injuries per year related to team or individual sport activities occurred to children and adolescents age 20 years and younger. Data reported is from consumer product-related injuries occurring in the United States from a statistically valid sample of emergency departments collected by the United States Consumer Product Safety Commission, National Electronic Injury Surveillance System. Data shown for sports injuries are not included in the overall total for musculoskeletal conditions among children and adolescents, on the assumption it duplicates numbers found in the emergency department database based on ICD-9-CM codes and used in the trauma injuries section.
Males report injuries at twice the rate as females (64% of injuries), with the highest number of injuries occurring in the junior high (10 to 13 years) and high school (14 to 17 years) ages. (Reference Table 7C.7.1 PDF [69] CSV [70])
Team sports, both organized and informal, accounted for just under one-half (46%, or 740,200 injuries) of all sports-related injuries reported. Basketball had the highest number of team sport related injuries at 33% and was closely followed by football at 31%.
Team sport injuries to males were three times the number reported for females (75%). The only sport in which female injuries outnumber male injuries is volleyball. Nearly half (45%) of team sport injuries to children and adolescents occurred during the high school years (age 14 to 17 years), with another 34% in the junior-high age range of 10 to 13 years. (Reference table 7C.7.1 PDF [69] CSV [70])
The most common musculoskeletal injury incurred was a sprain or strain, accounting for 47% of team sport injuries. Volleyball had the highest proportion of sprains and strains, followed by basketball. Baseball led in contusion injuries, while fractures occurred most frequently in football, followed by soccer and hockey (including field, ice, and roller hockey). Only 1% of team sport injuries were serious enough to result in hospitalization. (Reference table 7C.7.2 PDF [73] CSV [74])
Individual sports injuries accounted for 54% of total injuries reported (872,900). Almost one in five injuries (18%) occurred while riding bicycles or other nonmotorized wheeled equipment such as tricycles and scooters. These injuries occurred most frequently to children ages 10 to 13 years. Injuries on playground equipment were the second highest type of individual sport injuries, accounting for 15% of all injuries. Playground equipment injuries occurred almost exclusively to children younger than 14 years old and most commonly in children aged 5 to 9 years old. Skating injuries (which includes roller and ice skates, inline skates, and skateboards) were the cause of 11% of individual sport injuries.
Females accounted for a larger share of individual sport injuries (45%) than in team sports. Still, the only activities in which females had a significantly higher number of injuries than males were in gymnastics/cheerleading/dancing as well as track and field. (Reference Table 7C.7.1 PDF [69] CSV [70])
Fractures and sprains/strains each accounted for one-third of all individual sport activity injuries (36% and 36% respectively). However, the type of musculoskeletal injury varied substantially with the type of activity. Fractures resulted from playground equipment injuries more than one-half the time (57%), with a high share of fractures in snow sports (44%) and skating injuries (42%) as well. Sprains/strains occurred in almost two-thirds of track and field injuries (62%), and there were a higher share of sprains/strains occurring in fitness training (59%) and gymnastics/cheerleading/dancing (57%) as well. The most common type of injury reported from bicycle/wheeled equipment was contusions (44%). Nearly 3% of individual sport injuries resulted in hospitalization. (Reference table 7C.7.2 PDF [73] CSV [74])
Pediatric musculoskeletal neoplasms are relatively rare. They can be categorized as either benign or malignant, as has been done for this document. Musculoskeletal neoplasms are often also categorized by the type of tissue they produce or from which they are derived.
The most common types of tumors that affect the musculoskeletal system are cysts, bone-producing tumors, cartilage tumors, fibrous tumors, soft tissue tumors, and peripheral neuroectodermal tumors. Most benign tumors, such as nonossifying fibromas, result in little or no disability and require no treatment. Other benign tumors may require surgical intervention. Painful or prominent osteochondromas may require surgical excision. Simple bone cysts can weaken the bone, increase fracture risk, and may require surgical treatment in order to resolve the cyst and prevent or treat fracture. Other benign tumors include lipomas, fibrous dysplasia, enchondromas, osteoid osteoma, and osteoblastomas.
The most common malignant tumors of the pediatric musculoskeletal system are osteosarcoma, Ewing sarcoma/peripheral neuroectodermal tumor, rhabdomyosarcoma, and synovial cell sarcoma. Osteosarcoma is the most common malignant bone tumor in patients under 20 years of age, with an incidence of approximately 29 per 1 million people. Ewing sarcoma is the second most common pediatric malignant musculoskeletal tumor and is part of the Ewing family of tumors, which includes peripheral neuroectodermal tumors. Most of the tumors in the family have a genetic translocation.1 Long-term survival of patients with both tumors has drastically improved with the routine use of chemotherapy.
For additional information on musculoskeletal tumors in children, you can refer to the Tumors [84] section of this report.
Neoplasms, including both benign and malignant, were diagnosed in 155,500 children and adolescent healthcare visits in 2013, of which 43,100 had a primary diagnosis of a neoplasm. About one in seven (5%) of children and adolescents with any neoplasm diagnoses were hospitalized (23,000), but fewer than 1% of hospital discharges had a primary diagnosis of neoplasm (3,600). (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Slightly more males than females had a hospital discharge with any or a primary neoplasm diagnosis. For each year from birth until 18 years, there is an increasing incidence of neoplasm prevalence resulting in hospitalization.
Any diagnoses of neoplasm accounted for 4.4% of hospitalizations for any musculoskeletal condition diagnosis, and 0.4% of all hospitalizations for any healthcare condition. Hospitalizations with a primary diagnosis of neoplasm accounted for 0.7% of all musculoskeletal diagnoses and only 0.1% of hospitalizations for any health condition diagnosis. Benign neoplasms accounted for 59% of neoplasm diagnoses, but 87% of hospitalized diagnoses are malignant. (Reference Table 7C.8 PDF [87] CSV [88])
Total charges averaged $48,500 for a mean 4.6-day stay when children and adolescents were hospitalized with any diagnosis of neoplasm along with other medical conditions. With a primary neoplasm diagnosis, the stay was slightly longer (6.4 days), and mean charges were higher at $93,100. Mean length of stay was highest for children less than one year of age; however, hospital charges were highest for children ages 5 to 9 years old. Total hospital charges for primary neoplasm diagnosis discharges in 2013 were $335.2 million. (Reference Table 7C.8 PDF [87] CSV [88])
Skeletal dysplasias, also referred to as osteochondrodysplasias, are a heterogeneous group of disorders that affect the growth and development of bone and cartilage. There is great variability of severity and involvement ranging from neonatal lethality to mild growth differences noted incidentally in adulthood. Hundreds of such dysplasias have been described, but most are so rare that true incidence is difficult to estimate.1 The most common diagnoses included in this category are chondrodysplasia, achondroplasia, hypochondroplasia, dwarfism, congenital absence of rib, osteogenesis imperfecta, osteopetrosis, as well as other dysplasias. The overall incidence of skeletal dysplasias is two to five per 10,000 live births.2 Despite their relative rarity, many patients with these disorders require extensive medical and surgical treatments throughout their childhood and into adulthood.
Skeletal dysplasias were diagnosed in 235,800 children and adolescent healthcare visits in 2013, accounting for the primary diagnosis in 47,500 of these visits. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Males were slightly more likely to be hospitalized for both any musculoskeletal diagnosis as well as a primary diagnosis of dysplasia. Children from age 1 to 4 were most likely to be hospitalized with any diagnosis while children from 1 to 4 years and 10 to 17 years were equally likely to be hospitalized with a primary diagnosis of skeletal dysplasia. (Reference Table 7C.9 PDF [93] CSV [94])
Skeletal dysplasias as a primary diagnosis accounted for 0.3% of hospitalizations for any musculoskeletal diagnosis and 0.02% of hospitalizations for any condition. However, it is often the case that the primary diagnosis would reflect the problem associated with the condition rather than the condition itself. For example, with platyspondyly (flattened spinal bones), curvature of the lower back (lordosis) would be the diagnosis rather than dysplasia.
Total charges averaged $106,100 for a mean 10-day stay when hospitalized with a diagnosis of skeletal dysplasia with other medical conditions. With a primary diagnosis of skeletal dysplasia, the average stay was 8.6 days and cost $96,500. Mean length of stay and charges were highest in neonates. Total charges in 2013 were $144.8 million. (Reference Table 7C.9 PDF [93] CSV [94])
An estimated 300,000 children in the Unites States are diagnosed with juvenile arthritis or another chronic rheumatologic condition such as systemic lupus erythematosus, juvenile dermatomyositis, or linear scleroderma.1 These conditions generally require chronic care and, without appropriate treatment, can lead to significant disability.
Juvenile idiopathic arthritis (JIA) (formally called juvenile rheumatoid arthritis [JRA] or juvenile chronic arthritis [JCA]) is estimated to affect 1 in 1,000 children in the United States.2 JIA is diagnosed in a child younger than 16 years of age with at least six weeks of persistent arthritis. There are seven distinct subtypes, each having a different presentation and association to autoimmunity and genetics.3 Certain subtypes are associated with an increased risk of inflammatory eye disease (uveitis). Understanding the differences in the various forms of JIA, their causes, and methods to better diagnose and treat these conditions in children is important to future treatment and prevention. Among all subtypes, approximately half of children with JIA still have active disease after 10 years.4
There are several other causes of acute or chronic arthritis in children that do not meet the diagnostic criteria of JIA, including, but not limited to, rheumatic fever, Reiter syndrome/reactive arthritis, and the arthritis associated with inflammatory bowel disease.
Approximately 15% to 20% of cases of systemic lupus erythematosus (SLE) in the United States occur in children younger than 18 years of age. SLE is a chronic autoimmune condition characterized by the production of autoantibodies leading to immune complex formation and end organ damage. For reasons that remain unclear, pediatric SLE is associated with increased disease severity, increased short- and long-term morbidity, and mortality as compared to adult-onset SLE.5
Juvenile dermatomyositis is a chronic inflammatory condition characterized by inflammation of the skin and muscle. Estimated incidence of the disease in the United States is 0.5 per 100,000 people; the prevalence is not known.2
The sclerodermatous conditions are defined in part by the common clinical feature of tightening or hardening of the skin. Systemic scleroderma, also called diffuse cutaneous systemic scleroderma, is rare in childhood, accounting for only 2% to 3% of all cases of this condition, which has an estimated prevalence of 24 cases per 100,000 people. Linear scleroderma is the most common subtype of scleroderma diagnosed in the pediatric population. It is characterized by a linear streak of sclerosis typically involving an upper or lower extremity. 2
In 2006, the CDC Arthritis Program finalized a case definition for ongoing surveillance of pediatric arthritis and other rheumatologic conditions (SPARC) using the current ICD-9-CM diagnostically based data systems.6 In response to the variations in conditions that some felt should be included but were not, CDC generated estimates are not included in the case definition.
Rheumatologic conditions were diagnosed in 529,500 children and adolescent healthcare visits in 2013, of which 390,400 had a primary diagnosis of a rheumatologic condition. Only 2% of children and adolescents with any rheumatologic diagnoses were hospitalized (11,900), while less than 1% (3,700) with a primary diagnosis of a rheumatologic condition had a hospital discharge. Over one-half (58.3%) of children and adolescents with a rheumatologic condition diagnosis were seen in physicians’ offices. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Females were hospitalized with a rheumatologic condition at nearly three times the rate of males, both for any diagnoses and as a primary diagnosis. As children age, there is a higher incidence of a rheumatologic condition diagnosis.
Any diagnoses of a rheumatologic condition accounted for 2.4% of hospitalizations for any musculoskeletal condition diagnosis, and 0.2% of all hospitalizations for any healthcare condition. Hospitalizations with a primary diagnosis of a rheumatologic condition were 0.7% of all musculoskeletal diagnoses and 0.1% of hospitalizations for any health condition diagnosis. (Reference Table 7C.10 PDF [99] CSV [100])
Total charges averaged $47,500 for a mean 5.1-day stay when children and adolescents were hospitalized with any diagnosis of a rheumatologic condition along with other medical conditions. With a primary rheumatologic diagnosis, the stay was shorter (4.4 days), and mean charges slightly lower at $42,500. Males as well as children 18 to 20 years old had slightly longer average hospital stays and average hospital charges. Total hospital charges for primary rheumatologic condition diagnosis discharges in 2013 were $157.3 million. (Reference Table 7C.10 PDF [99] CSV [100])
Many medical problems have musculoskeletal implications. This section discusses some of the more common of those diagnoses, including hemophilia, sickle cell disease, and endocrine and metabolic disorders such as rickets and lysosomal storage disorders.
Hemophilia is a genetic disorder characterized by abnormal blood clotting secondary to congenital deficiency of clotting factors VIII or IX. It may result in musculoskeletal problems by way of intramuscular hemorrhage and hemophilic arthropathy. Hemophilic arthropathy occurs through spontaneous bleeding into a weight-bearing joint, resulting in cartilage degeneration and arthrosis as well as asymmetric growth stimulation and deformity.
Sickle cell disease is inherited in an autosomal dominant fashion and is characterized by production of abnormal hemoglobin. This results in reduced oxygen delivery to tissues and can lead to multiple musculoskeletal manifestations, including painful bone infarcts, osteomyelitis, avascular necrosis, and vertebral compression fractures.
Metabolic bone diseases, such as rickets, occur due to abnormal calcium and phosphate metabolism. Rickets occurs in many forms, including vitamin D deficiency, vitamin D resistance, hypophosphatemia rickets, and renal osteodystrophy. Regardless of the cause, the result is inadequate calcification of bone and cartilage, resulting in bone pain and deformity.
The most common lysosomal storage disease is Gaucher’s disease, an autosomal recessive condition characterized by a deficiency in the enzyme beta-glucocerebrosidase. In Gaucher’s disease, there is an accumulation of glucocerebrosides, which contain glucose, in the tissues. This results in musculoskeletal manifestations that include bone deformity secondary to bone marrow infiltration, avascular necrosis, bone pain, pathologic fracture, and osteomyelitis.
Medical problems with musculoskeletal implications were diagnosed in 566,700 children and adolescent healthcare visits in 2013, of which 24% (134,000) had a primary diagnosis of a medical problem with musculoskeletal implications condition. One in ten children and adolescents with any medical problem diagnoses were hospitalized (54,700), while 3.5% (4,700) with a primary diagnosis had a hospital discharge. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Males and females were hospitalized with a medical problem with musculoskeletal implications in about the same numbers, but with a primary diagnosis, males were more likely to be hospitalized. The highest rate of hospitalization, when compared to other MSK conditions, was for adolescents age 14 to 20 years of age.
Any diagnoses of a medical problem with musculoskeletal implications accounted for 10.9% of hospitalizations for any musculoskeletal condition diagnosis, and less than 1% of all hospitalizations for any healthcare condition. Hospitalizations with a primary diagnosis of a medical problem with musculoskeletal implications were less than 1% of all musculoskeletal diagnoses and 0.1% of hospitalizations for any health condition diagnosis. However, it is often the case that the primary diagnosis would reflect the problem associated with the condition rather than the condition itself. For example, a child with rickets is going to be hospitalized for a lower extremity deformity rather than for rickets. (Reference Table 7C.11 PDF [108] CSV [109])
Rickets accounted for 45.5% of all healthcare visits for medical problems with musculoskeletal implications, but 72% of the hospitalized cases. (Reference Table 7C.1.1 PDF [18] CSV [19])
Total charges averaged $119,200 for a mean 11.9-day stay when children and adolescents were hospitalized with any diagnosis of a medical problem with musculoskeletal implications along with other medical conditions. With a primary medical problem with musculoskeletal implications diagnosis, the stay was shorter (3.2 days), and mean charges about a fourth that of medical problems as a contributing condition ($29,500).
When hospitalized with any diagnosis of a medical problem with musculoskeletal implications along with other medical conditions, neonates and children less than 1 year of age had significantly longer stays and higher charges than other age groups, primarily due to cases of rickets. Total hospital charges for primary medical problem with musculoskeletal implications diagnosis discharges in 2013 were $138.7 million. (Reference Table 7C.11 PDF [108] CSV [109])
Musculoskeletal pain syndromes, including amplified musculoskeletal pain or juvenile fibromyalgia, chronic regional pain syndrome (reflex sympathetic dystrophy), benign hypermobility, and benign limb pains, are common diagnoses in the pediatric population. A systematic review examining the prevalence of chronic musculoskeletal pain found a range of prevalence rates between 4% and 40% in children. Rates were generally higher in girls and increased with age.1 It is estimated that 5% to 8% of new patients presenting to North American pediatric rheumatologists have a musculoskeletal pain syndrome.2
Amplified musculoskeletal pain can be localized or diffuse. Diffuse pain involving at least three major body parts for at least 3 months is seen in the diffuse type. Fibromyalgia is a subset of diffuse amplified musculoskeletal pain. Patients also typically have sleep disturbance and other somatic complaints, such as headaches and abdominal pain. Reflex sympathetic dystrophy (RSD), now called complex regional pain syndrome (CRPS), is a form of amplified pain in which autonomic dysfunction develops in an extremity, often following injury or trauma. The affected limb becomes swollen, discolored, and cold, and the area can be very painful with light touch (allodynia). The recommended treatment for these conditions includes restoring normal sleep patterns, a therapy program with a focus on exercise and desensitization, and cognitive behavioral therapy. Some patients require treatment in an in-patient setting. For further information see Childhood RND Educational Foundation, Inc., available at StopChildhoodPain.org [114].
Benign limb pains, sometimes referred to as “growing pains,” are most common in children age 2 to 5 years. Children with benign limb pains tend to complain of pain at night, often awaking from sleep due to pain. These symptoms tend to resolve with age.
Benign hypermobility is diagnosed in patients who have hypermobile joints3, without an underlying connective disuse disorder. This condition is common, affecting 8% to 20% of White populations. Anterior knee pain and back pain are more common in hypermobile vs non-hypermobile individuals.2
Pain syndromes were diagnosed in more than 2.7 million children and adolescent healthcare visits in 2013, of which 63% (1.8 million) had a primary diagnosis of a pain syndrome. Less the 1% of children and adolescents with any pain syndrome diagnoses were hospitalized (20,000), while a tiny fraction (1,700) with a primary diagnosis had a hospital discharge. Two-thirds (65%) of children and adolescents with a pain syndrome diagnosis were seen in physicians’ offices. (Reference Table 7C.1.1 PDF [18] CSV [19] and Table 7C.1.2 PDF [24] CSV [25])
Females were hospitalized with a pain syndrome diagnosis in slightly higher numbers than males, both for any diagnoses and as a primary diagnosis. Pain syndrome diagnoses increase as a contributing diagnosis in older children, but as a primary diagnosis was greatest between 14 and 17 years old followed by 5 to 13 years old.
Any diagnoses of pain syndrome accounted for just over 4% of hospitalizations for any musculoskeletal condition diagnosis, and 0.3% of all hospitalizations for any healthcare condition. Hospitalizations with a primary diagnosis of pain syndrome were 0.3% of all musculoskeletal diagnoses and a tiny portion of hospitalizations for any health condition diagnosis. (Reference Table 7C.12 PDF [117] CSV [118])
Total charges averaged $48,900 for a mean 6.1-day stay when children and adolescents were hospitalized with any diagnosis of a pain syndrome along with other medical conditions. With a primary pain syndrome diagnosis, the stay was shorter (3.1 days), and mean charges about half that of pain syndrome as a contributing condition ($25,800).
Sex was not a significant factor in length of hospital stay and average charges for a medical problem with a musculoskeletal pain syndrome diagnosis. In patients with a primary diagnosis of a pain syndrome, the average length of hospital stays (4.5 days) and average cost ($40,000) was highest among patients ages 10 to 13. Total hospital charges for primary pain syndrome diagnosis discharges in 2013 were $43.9 million. (Reference Table 7C.12 PDF [117] CSV [118])
An estimated 25,000 patients were seen in hospitals and emergency departments in 2013 for treatment of developmental dysplasia (DDH) of the hip.1 While DDH can often be successfully treated in childhood, it is now understood that even with successful treatment, residual effects can have a huge impact on the musculoskeletal burden of osteoarthritis in adulthood. One in four people are likely to develop symptomatic hip osteoarthritis in their lifetime.2 Thus, total hip arthroplasty is one of the most common musculoskeletal surgeries performed in the United States, with 343.6 thousand procedures performed in 2013.3 It is now also recognized that the underlying etiology of hip arthritis is often related to childhood developmental hip conditions such as Developmental Dysplasia of the Hip, Legg Calves Perthes disease, and Slipped Capital Femoral Epiphysis.4 A United States study of patients less than 50 years of age noted radiographic findings of developmental dysplasia of the hip in 23%.5. Long term outcome studies of surgeries to treat residual hip dysplasia in adults shows 74% native hip survival at 18 years.6 This long term impact of developmental hip conditions and the ability of hip hip preservation surgeries to prevent or delay onset of arthritis underscore the importance of early diagnosis and long term follow up into adulthood.
Other conditions commonly thought of as only affecting children, such as cerebral palsy, osteogenesis imperfecta, and spina bifida, are now being seen more than ever in adults thanks to the tremendous progress in care leading to longer life expectancy. Remarkably, some people with Duchenne’s muscular dystrophy are now surviving into early adulthood. Concomitant with this success has come a host of new issues concerning the transition of care to adulthood and the aging process.
Adults with these conditions are disproportionately affected by the aging process. Some issues are clear. For example, those with mobility challenges have difficulty participating in fitness regimens, leading to more sedentary lifestyles and secondary issues such as obesity, diabetes, and heart disease. Other issues are less clear. Adults with aftereffects of childhood musculoskeletal disorders have more difficulty accessing preventative care. Even more subtle are issues related to lack of providers skilled in treating adults with the sequela of childhood issues and psychosocial challenges.
The medical community needs to investigate whether the needs of patients are being met and if they are reaching full potential as productive adults. The margin of function which allows individuals to live independently is often very small. Early or more pronounced reduction in function associated with aging may make the difference in whether a care giver is required for activities of daily living or there is independent living.
Research into the Health-Related Quality of Life, prevalence of disease, potential to avoid disease, and availability of care, including preventative care, is required.
In 2013, total hospital charges for children and adolescents age 20 years and younger with a primary musculoskeletal-related diagnosis were $7.4 billion. Musculoskeletal trauma (41%) and deformity (37%) were the major contributors to total hospital charges, but all conditions contribute to the overall economic impact of musculoskeletal conditions in this age group. Furthermore, while musculoskeletal condition hospital charges represent 5.2% of total charges for all medical conditions for the age 20 years and younger age group, the number of discharges represent only 2% of total hospital discharges for any medical condition in this age group, indicating that musculoskeletal conditions may be more expensive to treat than many other childhood conditions. (Reference Table 7C.13 PDF [123] CSV [124])
It is important to note that the overall cost of musculoskeletal conditions in the 20 years and younger population is much greater than just hospital charges. First, the $7.4 billion includes only hospitalizations with a primary, or first, diagnosis in the databases, representing less than 2% of 2013 healthcare visits with any musculoskeletal condition diagnosis. Not included in this burden are expenditures for visits to emergency departments, outpatient clinics, and physicians’ office, as well as other medical care expenditures such as physical therapy, rehabilitation, and medications.
While gender is not a factor in the distribution of hospital charges, age is a major contributor. Children in the middle years of childhood, especially ages 10 to 13 years, have a higher share of total hospital charges (16%) due to musculoskeletal conditions than any other age group. Musculoskeletal condition hospital charges are also a higher share for those age 14 to 17 years (14%) and ages 5 to 9 years (8.6%).
To fully understand the burden of musculoskeletal diseases on children and adolescents, it is mandatory that data be available on prevalence, healthcare needs, cost associated with treatment, limitations due to musculoskeletal conditions, and overall impact these conditions have on the lives of children and adolescents. The HCUP KID, HCUP NIS, and HCUP NEDS databases provide a tremendous asset in understanding hospitalizations for this analysis, but they, too, have limitations. First among these is the inability to truly determine primary cause for visits, as multiple diagnosis codes may be included with each record, with no way of knowing which is the primary diagnosis. In addition, many healthcare visits are to a physician’s office, and the database for these visits National Ambulatory Medical Care Survey (NAMCS) is small and often contains insufficient cases (<35) for reliable analysis even when merging several years of data. This is particularly true for the very young patients (0 to 5 years) and for rare conditions. Injuries occur in enough numbers that this is not a problem. However, many other conditions had low numbers.
A second key challenge is ensuring that children with chronic medical and musculoskeletal problems have access to care, particularly for those with Medicaid or other government-funded insurance. Low physician reimbursement by government insurance results in fewer physicians who are willing or able to care for these patients, making access to needed specialty care difficult. Additionally, pediatric subspecialists who take care of musculoskeletal conditions are typically located at large children’s hospital in more populous cities, further reducing access to care for those in rural areas. Because of the unique nature of pediatric musculoskeletal problems and treatments, many adult subspecialists who may be more accessible are unable or unwilling to treat pediatric patients.
A third challenge is the need to track pediatric patients into adulthood to determine lifelong burden of their pediatric musculoskeletal disease. Once a child turns 18 years, the system loses them as they become more mobile and move on to other caregivers. Further, they may lose parental insurance or their Medicaid coverage. A better way to obtain long-term follow-up on their history and long-term outcomes of treatment of pediatric musculoskeletal disease is needed.
Poor bone health is being recognized as a key problem in pediatric musculoskeletal disease, one that will last a lifetime. Key factors leading to poor bone health are Vitamin D deficiency and childhood obesity. The current healthcare data system makes it very difficult to quantify the burden of these problems because they are infrequently evaluated as the primary diagnosis. Additionally, patients are rarely admitted or discharged for treatment specific for these diagnoses. In the future, methods for estimating the incidence of these diagnoses more accurately and assessing their contribution to musculoskeletal disease is necessary. Education of the individual, family, and society about the burden of obesity and Vitamin D deficiency is necessary to improve overall bone health in the United States.
Quality of life assessments in children and adolescents that allow better measure of the personal impact of pediatric musculoskeletal disease is lacking. In assessment of musculoskeletal disease for adults, lost wages and lost workdays are used to quantify burden. There is no corresponding way to measure burden in children. Currently, it is quantified indirectly by measuring lost wages and lost workdays for the child’s caregiver. Better methods for quantifying indirect burden of pediatric musculoskeletal disease is needed.
Better long-term follow-up data on pediatric musculoskeletal conditions is needed. Once patients reach adulthood, it becomes difficult for the physician who cared for their musculoskeletal conditions to keep track of them. This results in difficulty understanding adult manifestations of pediatric musculoskeletal conditions. On a global basis, the disability-adjusted life year (DALY), developed in the 1990s as a way of comparing the overall health and life expectancy of different countries, is used as a measure of overall disease burden expressed as the number of years lost due to ill-health, disability or early death. Disabilities incurred in childhood, expressed in the DALY, would provide greater understanding of the lifelong burden of these conditions.
MUSCULOSKELETAL INFECTIONS
Osteomyelitis: 730.0, 730.1, 730.2, 730.8, 73090, 73091, 73092, 73093, 73094, 73095, 73096,73097
Septic arthritis: 711.0, 711.4
Soft tissue infections (infective myositis): 72800, 72886
Lyme disease: 08881
Tuberculosis: 015
DEFORMITY
Upper Extremity:
Polydactyly: 75500, 75501
Syndactyly: 75510, 75511, 75512
Reduction deformities: 755.2
Other congenital anomalies upper limb: 755.5, 736.0, 736.1, 736.2, 73690, 75489, 75681, 75689
Lower Extremity:
Polydactyly: 75502
Syndactyly: 75513, 75514
Reduction deformities: 755.3
Other congenital anomalies lower limb: 755.6
Congenital deformities: 754.4, 754.59, 754.6, 754.7, 72781, 73400, 736.7, 736.8
Hip and Pelvis:
Congenital deformity of hip joint: 75561, 75562, 75563
Hip joint acquired: 736.3, 73220, 73860
Developmental dysplasia: 754.3
Spine and Pelvis:
Of spinal cord: 742.5
Of vertebral column: 737, 73850, 73200, 75420, 756.1
Other and Unspecified:
Congenital deformities: 754.8, 75540, 75580, 75590, 75682, 75690, 75689
TRAUMA: Fractures, dislocation, sprains and strains, open wound, crushing injury, contusion, traumatic compartment syndrome, unspecified injuries, injuries to nerve roots and spinal plexus
Upper Extremity: 810, 811, 812, 813, 814, 815, 816, 817, 818, 819, 831, 832, 833, 834, 840, 841, 842, 880, 881, 882, 883, 884, 885, 886, 887, 90520, 923, 927, 95891, 95920, 95930, 95940, 95950
Lower Extremity: 820, 821, 822, 823, 824, 825, 826, 827, 828, 829, 836, 837, 838, 844, 845, 90530, 90540, 924, 928, 95960, 95970, 95892
Hip and Pelvis: 835, 843, 84850, 808, 959.1, 953
Spine and Trunk: 805, 806, 807, 846, 847, 809, 875, 876, 90510, 92200, 92210, 92230, 92231, 92232, 92233, 92280, 92290, 926.1, 92680, 92690, 952
Birth Trauma: 767
Child Abuse: 995.5
NEUROMUSCULAR CONDITIONS
Cerebral palsy (CP): 343
Spina bifida (SB): 741
Muscular dystrophy (MD): 359
Charcot-Marie-Tooth disease (CMT): 35610, 35620
Other: 334, 335, 33600, 336
SYNDROMES WITH MUSCULOSKELETAL IMPLICATIONS
Marfan sydrome/Ehlers Danlos syndrome/other connective tissue disorders: 75982, 75683
Down's syndrome: 75800
Neurofibromatosis (NF): 23770, 23771, 23772
SPORTS INJURIES (Sports injuries data is from NEISS and does not use ICD-9 codes.)
SKELETAL DYSPLASIAS
Dysplasias: 75989, 65580, 73399, 39330
Chondrodystrophy/achondroplasia/hypochondroplasia: 75640
Dwarfism (thanatophoric dysplasia): 25940, 75651
Congenital absence rib: 75630
Osteogenesis imperfecta: 75651
Osteopetrosis: 75652
Other: 75654, 75655, 75656, 75659
NEOPLASMS
Benign:
Benign lesion of bone/cartilage: 213
Lipoma: 21400, 21410, 21420, 21430, 21480, 21490
Benign lesion of CT/ST: 215
Malignant:
Malignancy of bone/cartilage: 170
Malignancy of CT/ST: 171
RHEUMATOLOGIC CONDITIONS
Rheumatic fever: 39000, 39092
Reactive arthritis/Reiter disease (underlying disease, no principal diagnosis): 711.1
Juvenile idiopathic arthritis: 714.3
Ankylosing spondylitis and inflammatory spondylopathies: 720
Psoriatic arthritis: 696
Arthropathy of inflammatory bowel disease: 71310
Systemic lupus erythematosus: 71000
Juvenile dermatomyositis: 71030
Localized scleroderma: 70100, 71010
MEDICAL PROBLEMS WITH MSK IMPLICATIONS
Hemophilia: 00286
Sickle cell: 28260
Endocrine and metabolic disorders: 75650
Gaucher disease (lipidoses/lysosomal storage disorders): 27270
Osteoporosis: 733.0
Hyperthyroid (thyrotosicosis w/wo goiter): 242
Rhabdomyolysis: 72888
Other conditions: 28610, 25890
Rickets (Vitamin D deficiency, phosphorus, and calcium metabolism disorders): 268, 275.3, 275.4
PAIN SYNDROMES
Amplified musculoskeletal pain/Juvenile primary fibromyalgia syndrome: 30789, 72910
Reflex sympathetic dystrophy (complex regional3722 pain syndrome/CRPS): 337.2
Benign hypermobility/hypermobility syndrome: 72850
Benign limb pains (“growing pains”): 719.4
Links:
[1] https://www.cdc.gov/nchs/nhis/index.htm?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fnchs%2Fnhis.htm
[2] https://bmus.latticegroup.com/docs/bmus_4e_t7c.0.pdf
[3] https://bmus.latticegroup.com/docs/bmus_4e_t7c.0.csv
[4] https://bmus.latticegroup.com/docs/bmus_4e_t7c.0.1.pdf
[5] https://bmus.latticegroup.com/docs/bmus_4e_t7c.0.1.csv
[6] https://bmus.latticegroup.com/file/bmus4eg7c01png
[7] https://bmus.latticegroup.com/docs/bmus_4e_g7c.0.1.png
[8] https://bmus.latticegroup.com/docs/bmus_4e_t7c.0.2.pdf
[9] https://bmus.latticegroup.com/docs/bmus_4e_t7c.0.2.csv
[10] https://bmus.latticegroup.com/file/bmus4eg7c02png
[11] https://bmus.latticegroup.com/docs/bmus_4e_g7c.0.2.png
[12] https://www.boneandjointburden.org/fourth-edition/viic17/children-and-adolescent-icd-9-cm-codes
[13] https://www.hcup-us.ahrq.gov/
[14] https://bmus.latticegroup.com/file/bmus4et7c10jpg
[15] https://bmus.latticegroup.com/docs/bmus_4e_t7c.1.0.jpg
[16] https://www.cpsc.gov/cgibin/NEISSQuery/home.aspx
[17] http://report.nih.gov/fundingfacts/fundingfacts.aspx
[18] https://bmus.latticegroup.com/docs/bmus_4e_t7c.1.1.pdf
[19] https://bmus.latticegroup.com/docs/bmus_4e_t7c.1.1.csv
[20] https://bmus.latticegroup.com/file/bmus4eg7c11png
[21] https://bmus.latticegroup.com/docs/bmus_4e_g7c.1.1.png
[22] https://bmus.latticegroup.com/file/bmus4eg7c12png
[23] https://bmus.latticegroup.com/docs/bmus_4e_g7c.1.2.png
[24] https://bmus.latticegroup.com/docs/bmus_4e_t7c.1.2.pdf
[25] https://bmus.latticegroup.com/docs/bmus_4e_t7c.1.2.csv
[26] https://bmus.latticegroup.com/file/bmus4eg7c13png
[27] https://bmus.latticegroup.com/docs/bmus_4e_g7c.1.3.png
[28] https://bmus.latticegroup.com/file/bmus4eg7c14png
[29] https://bmus.latticegroup.com/docs/bmus_4e_g7c.1.4.png
[30] https://bmus.latticegroup.com/docs/bmus_4e_t7c.2.pdf
[31] https://bmus.latticegroup.com/docs/bmus_4e_t7c.2.csv
[32] https://bmus.latticegroup.com/file/bmus4eg7c21png
[33] https://bmus.latticegroup.com/docs/bmus_4e_g7c.2.1.png
[34] https://bmus.latticegroup.com/file/bmus4eg7c22png
[35] https://bmus.latticegroup.com/docs/bmus_4e_g7c.2.2.png
[36] https://bmus.latticegroup.com/docs/bmus_4e_t7c.3.pdf
[37] https://bmus.latticegroup.com/docs/bmus_4e_t7c.3.csv
[38] https://bmus.latticegroup.com/file/bmus4eg7c33png
[39] https://bmus.latticegroup.com/docs/bmus_4e_g7c.3.3.png
[40] https://bmus.latticegroup.com/file/bmus4eg7c31png
[41] https://bmus.latticegroup.com/docs/bmus_4e_g7c.3.1.png
[42] https://bmus.latticegroup.com/file/bmus4eg7c32png
[43] https://bmus.latticegroup.com/docs/bmus_4e_g7c.3.2.png
[44] https://www.aafp.org/afp/2014/1215/p843.html
[45] https://bmus.latticegroup.com/docs/bmus_4e_t7c.4.pdf
[46] https://bmus.latticegroup.com/docs/bmus_4e_t7c.4.csv
[47] https://bmus.latticegroup.com/file/bmus4eg7c41png
[48] https://bmus.latticegroup.com/docs/bmus_4e_g7c.4.1.png
[49] https://bmus.latticegroup.com/file/bmus4eg7c430png
[50] https://bmus.latticegroup.com/docs/bmus_4e_g7c.4.3.0.png
[51] https://bmus.latticegroup.com/file/bmus4eg7c42png
[52] https://bmus.latticegroup.com/docs/bmus_4e_g7c.4.2.png
[53] https://bmus.latticegroup.com/file/bmus4eg7c51png
[54] https://bmus.latticegroup.com/docs/bmus_4e_g7c.5.1.png
[55] https://bmus.latticegroup.com/docs/bmus_4e_t7c.1.5.pdf
[56] https://bmus.latticegroup.com/docs/bmus_4e_t7c.1.5.csv
[57] https://bmus.latticegroup.com/file/bmus4eg7c53png
[58] https://bmus.latticegroup.com/docs/bmus_4e_g7c.5.3.png
[59] https://bmus.latticegroup.com/file/bmus4eg7c52png
[60] https://bmus.latticegroup.com/docs/bmus_4e_g7c.5.2.png
[61] https://bmus.latticegroup.com/file/bmus4eg7c61png
[62] https://bmus.latticegroup.com/docs/bmus_4e_g7c.6.1.png
[63] https://bmus.latticegroup.com/docs/bmus_4e_t7c.6.pdf
[64] https://bmus.latticegroup.com/docs/bmus_4e_t7c.6.csv
[65] https://bmus.latticegroup.com/file/bmus4eg7c62png
[66] https://bmus.latticegroup.com/docs/bmus_4e_g7c.6.2.png
[67] https://bmus.latticegroup.com/file/bmus4eg7c71png
[68] https://bmus.latticegroup.com/docs/bmus_4e_g7c.7.1.png
[69] https://bmus.latticegroup.com/docs/bmus_4e_t7c.7.1.pdf
[70] https://bmus.latticegroup.com/docs/bmus_4e_t7c.7.1.csv
[71] https://bmus.latticegroup.com/file/bmus4eg7c72png
[72] https://bmus.latticegroup.com/docs/bmus_4e_g7c.7.2.png
[73] https://bmus.latticegroup.com/docs/bmus_4e_t7c.7.2.pdf
[74] https://bmus.latticegroup.com/docs/bmus_4e_t7c.7.2.csv
[75] https://bmus.latticegroup.com/file/bmus4eg7c73png
[76] https://bmus.latticegroup.com/docs/bmus_4e_g7c.7.3.png
[77] https://bmus.latticegroup.com/file/bmus4eg7c74png
[78] https://bmus.latticegroup.com/docs/bmus_4e_g7c.7.4.png
[79] https://bmus.latticegroup.com/file/bmus4eg7c75png
[80] https://bmus.latticegroup.com/docs/bmus_4e_g7c.7.5.png
[81] http://www.ncys.org/publications/2008-sports-participation-study.php
[82] http://www.physicalactivitycouncil.com/pdfs/current.pdf
[83] https://assets.aspeninstitute.org/content/uploads/2018/10/StateofPlay2018_v4WEB_2-FINAL.pdf
[84] https://www.boneandjointburden.org/fourth-edition/via0/tumors
[85] https://bmus.latticegroup.com/file/bmus4eg7c81png
[86] https://bmus.latticegroup.com/docs/bmus_4e_g7c.8.1.png
[87] https://bmus.latticegroup.com/docs/bmus_4e_t7c.8.pdf
[88] https://bmus.latticegroup.com/docs/bmus_4e_t7c.8.csv
[89] https://bmus.latticegroup.com/file/bmus4eg7c83png
[90] https://bmus.latticegroup.com/docs/bmus_4e_g7c.8.3.png
[91] https://bmus.latticegroup.com/file/bmus4eg7c82png
[92] https://bmus.latticegroup.com/docs/bmus_4e_g7c.8.2.png
[93] https://bmus.latticegroup.com/docs/bmus_4e_t7c.9.pdf
[94] https://bmus.latticegroup.com/docs/bmus_4e_t7c.9.csv
[95] https://bmus.latticegroup.com/file/bmus4eg7c91png
[96] https://bmus.latticegroup.com/docs/bmus_4e_g7c.9.1.png
[97] https://bmus.latticegroup.com/file/bmus4eg7c92png
[98] https://bmus.latticegroup.com/docs/bmus_4e_g7c.9.2.png
[99] https://bmus.latticegroup.com/docs/bmus_4e_t7c.10.pdf
[100] https://bmus.latticegroup.com/docs/bmus_4e_t7c.10.csv
[101] https://bmus.latticegroup.com/file/bmus4eg7c101png
[102] https://bmus.latticegroup.com/docs/bmus_4e_g7c.10.1.png
[103] https://bmus.latticegroup.com/file/bmus4eg7c102png
[104] https://bmus.latticegroup.com/docs/bmus_4e_g7c.10.2.png
[105] http://www.cdc.gov/arthritis/basics/childhood.htm
[106] https://bmus.latticegroup.com/file/bmus4eg7c111png
[107] https://bmus.latticegroup.com/docs/bmus_4e_g7c.11.1.png
[108] https://bmus.latticegroup.com/docs/bmus_4e_t7c.11.pdf
[109] https://bmus.latticegroup.com/docs/bmus_4e_t7c.11.csv
[110] https://bmus.latticegroup.com/file/bmus4eg7c112png
[111] https://bmus.latticegroup.com/docs/bmus_4e_g7c.11.2.png
[112] https://bmus.latticegroup.com/file/bmus4eg7c113png
[113] https://bmus.latticegroup.com/docs/bmus_4e_g7c.11.3.png
[114] https://stopchildhoodpain.org/
[115] https://bmus.latticegroup.com/file/bmus4eg7c121png
[116] https://bmus.latticegroup.com/docs/bmus_4e_g7c.12.1.png
[117] https://bmus.latticegroup.com/docs/bmus_4e_t7c.12.pdf
[118] https://bmus.latticegroup.com/docs/bmus_4e_t7c.12.csv
[119] https://bmus.latticegroup.com/file/bmus4eg7c122png
[120] https://bmus.latticegroup.com/docs/bmus_4e_g7c.12.2.png
[121] https://www.boneandjointburden.org/fourth-edition/iiib70/joint-pain-and-joint-replacement
[122] http://dx.doi.org/10.1007/s11999-016-4903-3
[123] https://bmus.latticegroup.com/docs/bmus_4e_t7c.13.pdf
[124] https://bmus.latticegroup.com/docs/bmus_4e_t7c.13.csv
[125] https://bmus.latticegroup.com/file/bmus4eg7c141png
[126] https://bmus.latticegroup.com/docs/bmus_4e_g7c.14.1.png
[127] https://bmus.latticegroup.com/file/bmus4eg7c142png
[128] https://bmus.latticegroup.com/docs/bmus_4e_g7c.14.2.png
[129] https://bmus.latticegroup.com/file/bmus4eg7c143png
[130] https://bmus.latticegroup.com/docs/bmus_4e_g7c.14.3.png