 [8]
[8] 

Spine disorders includes two major areas:
Low Back and Neck Pain [1] and Spinal Deformity [2].
Lumbar/low back pain and cervical/neck pain are among the most common medical conditions requiring medical care and affecting an individual’s ability to work and manage the daily activities of life. Back pain is the most common physical condition for which patients visit their doctor. In any given year, between 12% and 14% of the United States adult population age 18 and okder visit their physician with complaints of back pain. The number of physician visits has increased steadily over the years. In 2013, more than 57.1 million patients visited a physician with a complaint of back pain, compared to 50.6 million in 2010. (Reference Table 2A.5 PDF [3] CSV [4]) In addition, an unknown number of patients visit a chiropractor or physical therapist for these complaints.
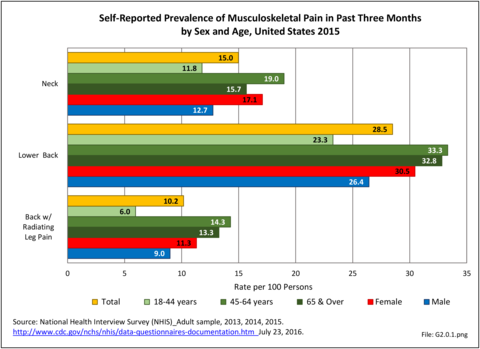
A large healthcare survey is conducted annually in the United States by the National Center for Health Statistics to identify the incidence and prevalence of select health conditions. On average, back pain was reported by 33.9% of persons aged 18 years and older for the years 2013-2015. Low back pain was the most common type of back pain, affecting 28.5%; neck pain was the second most common at 15.0%. The prevalence of back pain has remained stable since 20051 and is measured in response to the question of whether the individual “had low back pain or neck pain during the past three months.” Females report back pain more frequently than males (36.6% vs. 31.0%). The prevalence of low back pain and neck pain is highest for adults aged 65 years and over, but only slightly lower for adults aged 45-64. White, non-Hispanic adults are responsible for the highest prevalence of all back pain at 36.4%. When comparing geographic regions of the US, patients located in the Midwest report back and neck pain at the highest percentage (36.6%). (Reference Table 2A.1 PDF [5] CSV [6])
Approximately 1 in 17 persons (6.0%) of the population age 18 or older report they have a health condition that precludes work. Among these adults, 25.8%, or about 4 of the 17, are unable or limited in work due to chronic back or neck problems. (Reference Table 2A.11.1 PDF [11] CSV [12])
The estimated annual direct medical cost for all persons with a back-related condition in 2014 dollars was an average of $315 billion per year across the years 2012-2014. (Reference Table 8.6.2 PDF [13] CSV [14]) This is further discussed under the Economic Burden topic in this Spine section, and in the Economic Cost topic at this site. As noted previously and elsewhere, this is not the true cost because chiropractic care, physical therapy, alternative therapy, and other care is not included in the analysis. Also, treatment cost from outpatient clinics is currently not available; hence, these data are missing or incomplete.
Back pain often originates from sources that are not readily identifiable. Many causes of back pain are likely related to degenerative changes, but the actual underlying cause of a given back pain episode is often uncertain. In reviewing administrative data for prevalence, it is important to realize that the diagnostic categories may be inaccurate because they reflect differing interpretations about the source of the back pain rather than an absolute diagnosis. This will be discussed further in later sections.
For purposes of further analysis, we decided to divide the diagnostic codes defining the burden of spine problems into three groups: back disorders, disc disorders, and back injuries. This approach allows comparison to earlier editions of the text. We are aware there may be substantial overlap, and that some of the back disorders may be related to degenerative disc changes and some of the disc disorders may have another origin. The role of disc degeneration in the cause of back pain remains uncertain. Intervertebral disc degeneration and associated facet joint osteoarthritis seem to be a natural process of aging but can alter the biomechanics and function of the spine. Studies have identified a strong genetic predisposition, but there are modifying influences including age, obesity, smoking, and genetics.
In the tables and text, we define back disorders by diagnostic ICD-9-CM Codes 720, 721, and 724. These codes include inflammatory spine conditions, spondylosis, spinal stenosis, lumbago, sciatica, backache, and disorders of the sacrum. Disc disorders include herniations, disc degeneration, and post-laminectomy syndromes (ICD-9-CM Code 722). Back injuries include fractures, dislocations, and sprains (ICD-9-CM Codes 805, 806, 839, 846, and 847). The same classifications are used for both low back pain and neck pain. Thoracic back pain, or upper and middle back pain associated with the 12 spinal bones connected to and in the same level in the body as the 12 ribs, is less common and not as well studied. Data associated with thoracic spine pain is generally included in the analysis of low back back and disc disorders and injuries.
Unfortunately, the databases do not permit diagnostic verification. Sometimes diagnoses are provided primarily for reimbursement purposes, with little emphasis on accuracy. Further, there is considerable overlap. For example, a patient with back pain of unknown origin could be given the diagnosis of lumbago, placing him or her in the back disorder category. He or she may also have disc degeneration with a diagnosis of degenerative disc disease and, therefore, be placed in the disc disorder category. Or, if his or her problem developed after a lift or twist, it could be diagnosed as a back strain, falling into the back injury category.
In the tables and graphs, total healthcare visits include hospital discharges obtained from the 2013 Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample, emergency department visits obtained from the 2013 HCUP Nationwide Emergency Inpatient Sample, hospital outpatient visits obtained from the 2011 National Hospital Ambulatory Medical Care Survey Outpatients (NHAMCS-OP), and physician office visits obtained from the 2013 National Ambulatory Medical Care Survey (NAMCS).
Using the diagnostic code grouping discussed above, back disorders accounted for 82% of low back pain healthcare resource utilization in 2013. Back disorders accounted for 75% of hospitalizations. Disc disorders accounted for 16% of low back pain resource visits, and approximately 23% of hospitalizations. Emergency department visits for disc disorders were not common, comprising only 7% of all back pain-related visits. Back injuries, which include fractures, sprains, and strains, are often reported as caused by overexertion or overuse. They accounted for the remaining 12% of 2013 low back pain resource visits. Back injuries were most commonly seen in the emergency room (23%), but constituted only 8% of hospitalizations, indicating that most were manageable in an outpatient setting, and were most likely soft tissue injuries. (Reference Table 2A.2.1 PDF [15] CSV [16])
For each of the years 2013 to 2015, an annual average of nearly 29% of the US population age 18 years and older self-reported having had low back pain during the past three months. Among persons reporting low back pain, one in three (35.7%) suffered from back pain radiating into the leg. Approximately one-third of persons reporting low back pain also reported experiencing neck pain. Lower back pain is reported in higher rates by females (30.5%) than males (26.4%). The highest rates for lower back pain reported for both genders occurred in the 45-64 years age group (33.3%); there is a slight decrease in low back and neck pain complaints in ages 65 years and older (32.8%). Low back pain is most prevalently reported in the non-Hispanic white ethnic group. The Midwest region of the United States is responsible for recording the highest prevalence of low back pain. With the exception of persons 18 to 44 years, the prevalence of lower back pain with or without radiating leg pain did not vary considerably across all measured demographic categories. (Reference Table 2A.1 PDF [5] CSV [6])
As discussed previously, healthcare utilization by people with low back pain, which represents 82% of back pain healthcare visits, is only understood in part due to the lack of information about visits to chiropractors, physical therapists, and others involved in the care of back pain. Even so, the reported numbers in the databases are very high. In 2013, nearly 62 million visits to hospitals, emergency departments, outpatient clinics, and physician offices included a diagnosis of low back pain. Three in four visits were to physician offices, but more than 2.3 million patients were hospitalized and almost 10 million patients were treated for low back pain at an emergency department. (Reference Table 2A.2.1 PDF [15] CSV [16] and Table 2A.4.1 PDF [19] CSV [20])
The prevalence of low back pain healthcare visits is greatest in the 45-64 years age group, closely followed by the 18-44 years age group. Together, the 18-64 years age group represents 72% of all low back pain healthcare visits. However, adjusting for the 2013 US Census population estimates, healthcare visits for low back pain per 100 persons is highest in the 65 years and older age group, where it is 36.1%. In reviewing the three low back diagnostic categories, the category labeled "back disorders" dominates in all age groups. Disc disorders are uncommon in the younger than 18 years age group, but increase in frequency as the population ages, and are most prevalent in the 45-64 years age group. Back injuries are more common in patients younger than age 45 years (48%), declining to 14% in those 65 years and older. (Reference Table 2A.2.2 PDF [23] CSV [24])
The average age of persons hospitalized in 2013 for low back pain was 61.8 years. This compared to an average age of 47.2 years for persons visiting an emergency department, 49.4 years for visits to outpatient departments, and 54.5 years for visits to a physician. These numbers are essentially unchanged since 2010, with the exception of the average age of persons visiting an emergency department, which increased by 4.5 years. (Reference Table 2A.2.2 PDF [23] CSV [24])
Low back pain is found more frequently among females than males, with females representing 55% of healthcare resource visits. Back disorders, in particular, are more common in females, while disc disorders and back injuries are recorded similarly between sexes. Over 8 in 10 (84.4%) female healthcare visits in 2013 for low back pain were classified as back disorders, compared to 80.4% for males. This is probably a reflection of the prevalence of spinal stenosis and degenerative spondylolisthesis in both sexes. (Reference Table 2A.2.1 PDF [15] CSV [16])
Ethnic groups show preferences in where they might go to receive healthcare for low back pain, as exemplified by the rate of visits per 100 persons per race/ethnicity in the population. Overall, three out of four (74%) patients seen at a hospital were non-Hispanic whites, totaling approximately 1.8 million visits. This is in comparison to a combined total of 380,000 inpatient visits for non-Hispanic black (10%) and Hispanic (6%) visits. In contrast, for outpatient healthcare visits, non-Hispanic black (15%) and Hispanic (13%) ethnic groups reported an increase in percentage of visits compared to the hospital setting, a total of 1.2 million visits. Non-Hispanic white (66%) patients reported 2.8 million outpatient low back pain visits. Race/ethnicity is not reported in the NEDS database on emergency department visits. (Reference Table 2A.2.3 PDF [31] CSV [32])
Total healthcare visits for low back pain reflected differences between regions regarding back injuries (7.2 million) and back and disk disorders (50.9 million; 10 million). The southern United States recorded the highest percentage of total visits for back and disc disorders (31%; 40%), while the western United States recorded the highest percentage of total visits for back injuries (31%). (Reference Table 2A.2.4 PDF [33] CSV [34])
Persons hospitalized for low back pain in 2013 spent, on average, nearly 5 days in the hospital. Persons hospitalized for low back injuries were hospitalized for the longest period, an average of 6.8 days. When comparing the total days of hospitalization for all causes with those for low back pain are similar. As a proportion of hospitalizations for all causes, back pain constitutes 7% of both discharges and of total hospital days. The length of hospital stays has remained relatively stable since 2004. (Reference Table 2A.8 PDF [35] CSV [36] and Table 2A.9 PDF [37] CSV [38])
The mean length of stay for all low back pain discharges was similar between sexes. Regarding back injuries, length of stay of males is 1.5 days longer than for females (7.6 vs 6.1 days). (Reference Table 2A.10.1 PDF [39] CSV [40])
Age is an important factor influencing length of stay. Although they constitute a small proportion of back pain hospitalizations, persons younger than 18 years have longer stays for back pain, a ratio of 1.56 days longer, when compared to the average length of stay for all causes for this age group. After the age of 18 years, the length of hospital stays for back pain tend to increase as the population ages, however, similar patterns are seen with other diagnoses. (Reference Table 2A.10.2 PDF [41] CSV [42])
When comparing length of stay for all causes with those for low back pain, non-Hispanic white patient back pain visits compose 8% of both discharges and of total hospital days, approximately twice the proportion of discharges and of total hospital days reported by all other ethnic groups. However, the average length of stay tended to be slightly longer for non-Hispanic black (5.2 days) and Hispanic (5.1) patients than for non-Hispanic white patients (4.7 days). No considerable difference is observed in length of stay among geographic regions. (Reference Table 2A.10.3 PDF [43] CSV [44] and Table 2A.10.4 PDF [45] CSV [46])
Average hospital charges are provided along with length of stay in the HCUP NIS database. On average, hospital charges for a low back pain inpatient visit were 129% that of the average inpatient visit for any cause. In 2013, an estimated $120 million in charges were assessed against the 2.3 million inpatient stays for low back pain, 9% of the estimated total $1.2 billion in hospital charges for that year. Mean charges at $80,800 are highest for lumbar back injuries and, at $46,100, lowest for lumbar back disorders. When comparing male and female differences in the proportion of low back pain inpatient visit to total inpatient visit charges, no significant differences were found. Patients age 45-64 years and 65 years and older represent 83.7% of the total expenditure for low back pain hospital charges among the population. These age groups also demonstrate the highest proportion of total charges for all causes to those for low back pain, 10% on average. (Reference Table 2A.9 PDF [37] CSV [38]; Table 2A.10.1 PDF [39] CSV [40]; and Table 2A.10.2 PDF [41] CSV [42])
Variations in hospital charges by US geographic location are observed. The South region, whhich has the largest population, records the highest total hospital charges as well as total discharges among the geographic locations. Across ethnic groups, non-Hispanic white patients account for 76.7% of total charges for hospitalized persons with a diagnosis of back pain while comprising 65.5% of the population. However, the highest mean charges are found among thoses of Hispanic ethnicity. (Reference Table 2A.10.3 PDF [43] CSV [44] and Table 2A.10.4 PDF [45] CSV [46])
Cervical/neck pain is another common reason for visiting a doctor. In 2013, 21.4 million patient visits, or 1.8% of all healthcare visits to hospitals and physician offices, were for neck pain. Three out of four (73%) of these were physician visits, while only a small number (3%) of patients with neck pain were hospitalized. (Reference Table 2A.4.1 PDF [19] CSV [20])
Cervical disorders accounted for the majority (72%) of healthcare visits for neck pain in 2013. Neck disorders are primarily treated in outpatient clinics or physician offices but are also responsible for the highest percentage of hospital discharges (65%) for neck pain. Cervical disc disorders accounted for only 16% of all neck pain healthcare visits in 2013 but were responsible for one-third of hospitalizations (32%). Neck injuries accounted for 22% of all neck pain healthcare visits. This is a much higher percentage than that reported for low back injuries. Patients with neck injuries were primarily treated in an outpatient setting and represented 46% of all emergency department visits for neck pain and approximately one out of every five hospital outpatient and physician office visits. (Reference Table 2A.3.1 PDF [53] CSV [54])
The data on cervical/neck pain shows that hospital discharges are rare in people younger than age 18 years. When adjusted for the US 2013 Census population, estimates for hospital discharges are highest in the 45-64 years age group. The average age for persons hospitalized for neck pain was 59.8 years. Emergency department visits occurred most frequently in patients aged 18-44 years with an average age of 44.3 years. The average age of patients for hospital outpatient and physician office visits was 49.9 years and 51.9 years of age, respectively. (Reference Table 2A.3.2 PDF [57] CSV [58])
Almost four of five neck pain diagnoses (77.2%) in 2013 occurred in persons between ages of 18 and 64 years. Almost one in five patients (19.7%) were older than 65 years, and only 3.1% were younger than 18 years of age, although this group represents 24% of the US population. The diagnosis category of "cervical disorders" dominated over cervical disc disorders and cervical injury diagnoses categories among total healthcare visits for neck and cervical spine disorders in all age groups. When comparing age groups, patients younger than 18 and patients aged 18-44 years experienced a larger percentage of neck injuries relative to all neck pain visits, 33.3% and 36.4%, respectively. (Reference Table 2A.3.2 PDF [57] CSV [58])
In 2013, females accounted for 59% of the healthcare visits for neck pain overall, 59% of cervical disorder visits, and 62% of neck injury visits. Males accounted for 53% of the visits for cervical disc disorders. (Reference Table 2A.3.1 PDF [53] CSV [54])
Non-Hispanic black and Hispanic patients display differences in choice of healthcare utilization for neck pain. Non-Hispanic black patients account for 29% of all outpatient visits; 20% are treated in a hospital outpatient clinic and 9% are treated in the physician office setting. In contrast, although Hispanic patients utilize outpatient settings to a similar degree (32%), 14% receive treatment in a hospital outpatient setting and 18% receive treatment in a physician’s office. When evaluating total healthcare visits for neck pain, non-Hispanic white patients account for most of the visits (57%), followed by Hispanic and non-Hispanic black patients (14%; 8%). (Reference Table 2A.3.3 PDF [65] CSV [66])
When adjusted for the US 2013 Census population, estimates for hospital discharges for cervical disorders are similar throughout the four US regions analyzed, but were highest in the South region for emergency department visits (3% of all visits for any diagnoses) and in the West region for outpatient visits (2.7%) and physician office visits (2.3%). Overall, healthcare visits for cervical disorders are highest in the western United States, representing 2.1% of visits for any diagnoses. (Reference Table 2A.3.4 PDF [67] CSV [68])
Persons hospitalized for neck pain in 2013 spent an average of 4.6 days in the hospital. Those hospitalized for neck injuries had the longest stay, on average 7.2 days. When comparing total days of hospitalization for all causes with those for neck pain, the average length of stay is similar. Overall, hospitatl stays for neck pain constituted 2% of both discharges and total hospital days in 2013. The length of hospital stays has remained relatively stable since 2004. (Reference Table 2A.8 PDF [35] CSV [36] and Table 2A.9 PDF [37] CSV [38])
Although females are likely to have slightly shorter hospital stays for all causes of neck pain, it is only for neck injuries that a significant difference is seen: 8.0 days for males versus 6.2 days for females. (Reference Table 2A.10.1 PDF [39] CSV [40])
Age is a greater factor in length of stay than gender. Although persons younger than 18 years of age constitute a small proportion of back pain hospitalizations, they have, on average, a stay that is 1.62 times longer than the average length of stay for persons in this age group for all causes. Hospital stays for neck pain are consistent between ages 18 to 64 years at 4.2 days, increasing to 5.1 days in the 65 years and older age group. (Reference Table 2A.10.2 PDF [41] CSV [42])
Average length of stay for non-Hispanic white patients for all cervical/neck pain is 4.4 days compared with 5.2 days for non-Hispanic black, non-Hispanic other, and Hispanic patients. The length of stay for neck injuries is longer by a day or more for non-Hispanic black, non-Hispanic other, and Hispanic patients compared with non-Hispanic white patients (6.9 to ≥ 8.0) . There is no significant difference in length of stay among geographic regions. The southern region of the United States reports the highest number of discharges and total hospital days for all causes, but this region also has a larger share of the population. (Reference Table 2A.10.3 PDF [43] CSV [44] and Table 2A.10.4 PDF [45] CSV [46])
Average hospital charges are provided along with length of stay in the HCUP NIS database. Hospital charges are not what is actally paid, but the initial charges from the hospital, which provide a measure for comparison purposes. On average, hospital charges for a neck pain inpatient visit were 148% that of the average inpatient visit for any cause. In 2013, an estimated $36 million in charges were assessed against the 614,200 inpatient stays for neck pain, 3% of the estimated total $1.4 billion in hospital charges for that year. Mean charges of $97,400 were highest for neck injuries and, at $52,900, lowest for neck disorders. (Reference Table 2A.9 PDF [37] CSV [38])
In patients with neck pain, the 45-64 and 65 years and older age groups collectively represent 81.8% of the total hospital charges among the population. Of note, the ratio of mean charges for cervical/neck pain to all hospital charges is highest in ages 18 years and younger (3.24), decreasing as the population ages. No considerable differences are reported between males and females in relation to hospital charges. (Reference Table 2A.10.1 PDF [39] CSV [40] and Table 2A.10.2 PDF [41] CSV [42])
Hispanic patients show the largest ratio of mean hospital charges for neck pain-related visits to total hospital visits, at 1.91. This is in comparison to the ratio of 1.53 and 1.42 for non-Hispanic blacks and non-Hispanic whites, respectively. Non-Hispanic white patients account for 73.2% of total spending for neck pain visits, primarily because they compose a larger share of the total population. (Reference Table 2A.10.3 PDF [43] CSV [44])
There is only a slight variation among geographic regions with regard to the ratio of hospital charges for neck pain visits to total hospital visit charges, with the West region of the US displaying the largest ratio of 1.57 based on mean charges per visit of $81,200. The northeastern United States has the smallest ratio,1.36, indicating charges were closer to the overall US average. The Midwest region had the lowest mean charges per visit. Reference Table 2A.10.4 PDF [45] CSV [46])
As discussed on previous pages, back pain was the most common reason for healthcare visits among musculoskeletal disorders in 2013. In 2013, nearly 1 in 4 persons (24.7%) in the United States had a healthcare visit with a diagnosis of back pain, accounting for 6.4% of healthcare visits for any cause. Three out of four visits (73%) were physician office visits and the number of physician office visits for back pain continues to increase. In 1998 there were 32 million visits in 2004 nearly 45 million, and in 2013 more than 57 million. Physician office visits for back pain not only show a rapid increase in number, but also continue to include a larger share of the population. In 1998, 11.8 in 100 persons visited a physician because of back pain. In 2004, this had increased to 15.1 persons in 100. Although a slight decrease was seen through 2008, by 2013 the ratio had increased to 18.1 persons in 100. Low back pain accounted for most of the increase in visits. (Reference Table 2A.4.1 PDF [19] CSV [20] and Table 2A.5 PDF [3] CSV [4])
With respect to sex, females accounted for 58% of total back pain healthcare visits in 2013, however, the rate of total back pain visits per 100 patients was slightly less than that of males (6.4 vs. 6.5). Persons ages 45 to 64 years had the highest rate of total back pain diagnosis per 100 patient visits (9.5), but those aged 65 and older had the highest rate per 100 persons in their age group (43.7). The rate of total back pain visits per 100 patient visits was similar across all race/ethnic groups and geographic regions, with non-Hispanic whites and residents of the northeastern United States having the highest rates per 100 persons (23.2 and 29.5, respectively). (Reference Table 2A.4.1 PDF [19] CSV [20]; Table 2A.4.2 PDF [75] CSV [76]; Table 2A.4.3 PDF [77] CSV [78]; and Table 2A.4.4 PDF [79] CSV [80])
Most patients who present to a hospital emergency department with back pain are treated and routinely discharged to home from the emergency department (83.2%), with only a minority requiring admission to an inpatient unit (13.4%). These statistics are similar to all other emergency department discharges. When discharged from the hospital after a diagnosis of back pain, whether as a transfer patient from the emergency department or a direct hospital admission, routine discharges drop to about 60%, with 1 in 5 (22%-25%) discharged to another care facility and 13%-14% discharged with home health care. These numbers are somewhat higher than those found among all hospital discharges for any diagnoses. (Reference Table 2A.6 PDF [81] CSV [82])
No significant differences are observed in disposition of back pain visits to the emergency department or hospital between sexes, but females are slightly more likely to be discharged to another care facility or have home health care provided. When comparing age groups, a large majority of routine discharges are observed in patients aged 45 years or younger. The percentage of routine discharges is decreased by 10% to 82.6% for the 45 to 64 years age group, and is reduced by another 20% in the 65 years and older age group (60.6%). By age 65 and older, more than half of the discharges are to another care facility or with home health care. No meaningful differences are observed in the disposition of patients with respect to race/ethnicity. Residents of the Northeast region are the most likely to be discharged to additional care (40.5%). (Reference Table 2A.7.1 PDF [83] CSV [84]; Table 2A.7.2 PDF [85] CSV [86]; Table 2A.7.3 PDF [87] CSV [88]; and Table 2A.7.4 PDF [89] CSV [90])
Approximately 6% of the working age population, persons age 18 years and older, report they are unable to work or limited in the type of work they can perform because of a medical condition. Among this group, 25.8% reported they are unable to work due to back or neck problems. Similar ratios of limitations related to daily living are also found. Approximately 1 in 22 persons of working age has difficulty walking without equipment due to a medical condition; 24.8% report that condition to be back or neck pain. Overall, 13.5% of working-age persons report at least one limitation with activities of daily living, which include eating, preparing food, bathing, rising from a chair, walking up steps, etc. For one in five of these persons, the cause of their limitation is back or neck pain. (Reference Table 2A.11.1 PDF [11] CSV [12])
Age groups account for major differences in limitations due chronic back or neck problems. One in three patients age 65 years and older report they have limitations in activities of daily living (ADL), with 1 in 5 (19.2%) reporting ADL due to chronic back or neck pain. Among the 17% of persons with ADL for any cause in the 45 to 64 years age group, 29.9% list the cause is due to chronic back or neck problems. Of note, in this age group, chronic back or neck pain is the cause of each type of limitation, including inablity to work at all or type of work, for approximately 1 in 3 with limitations from any cause. No considerable differences are reported between males and females. (Reference Table 2A.11.1 PDF [11] CSV [12] and Table 2A.11.2 PDF [95] CSV [96])
Although the race/ethnic group classified as non-Hispanic others represents a small proportion of the total population, they report the lowest rates of limitations in activities of daily life. Hispanic patients report fewer limitations due to any health condition (9.8%) than non-Hispanic whites (15.1%) and non-Hispanic blacks (16.1%). Among persons with limitations due to any cause, non-Hispanic whites (20.8%) and non-Hispanic black patients (19.5%) have comparatively higher percentages of limitations due to chronic back or neck problems compared with Hispanic patients (15.1%), with the exception of difficulty walking without equipment. No significant differences are seen among geographic regions in ADL. (Reference Table 2A.11.3 PDF [97] CSV [98] and Table 2A.11.4 PDF [99] CSV [100])
Self-reported bed days and work days lost due to back or neck pain have fluctuated over the past decade. Both recorded their highest totals in 2008, registering 385,000 lost work days and 671,000 bed days. Both bed days and work days lost have remained steady since 2012. (Reference Table 2A.12 PDF [101] CSV [102])
Work days lost due to spine pain or spine problems were more frequently reported by females than males during 2015 (17.4% vs. 13.5%). However, females, on average, lose one less day of work than do men (9.9 to 11.2, respectively). (Reference Table 2A.13.1 PDF [103] CSV [104])
Back pain severe enough to keep people from working in any occupation is most likely to occur in the 18 to 64 years age group, accounting for 14.8% of persons in the 18 to 44 years age group, and 16.9% of persons in the 45 to 64 years age group. This is, of course, not surprising since those are the most common years in which people work. The average number of workdays lost was 8.6 and 12.5 days for the two age groups, respectively. The oldest group of workers, age 65 years and older, report more than 16 days of work lost due to spine pain or problems, but they constitute such a small group that their impact is less than that of younger workers. (Reference Table 2A.13.2 PDF [107] CSV [108])
When comparing ethnic groups, Hispanic persons record the highest average number of work days lost due to spine pain (14.1), followed by non-Hispanic whites and non-Hispanic blacks (10.1 days; 9.9 days). No meaningful difference by share of workforce is observed in average number of work days lost due to spine pain according to geographic region, but workers in the Northeast and Midwest regions of the US lose the most days, on average (11.6 and 12.1, respectively). (Reference Table 2A.13.3 PDF [109] CSV [110] and Table 2A.13.4 PDF [111] CSV [112])
The National Health Care Interview Survey also provides information about the incidence of bed days, days in which a person was in bed for a half day or more due to injury or illness, during 2015. The average number of bed days per worker for all spine pain or problems was 7.8 days. On average, males reported taking 8.5 bed days compared to 7.3 bed days taken by females. The percent of people in the workforce reporting bed days due to spine pain or problems is higher in the 18 to 44 years and 45 to 64 years age groups (13.8% and 15.3%, respectively) than for those age 65 and over. This is likely due to the health status of older workers, who tend to be healthy if they are still in the workforce. Between these two age groups, persons 45 to 64 take approximately 3 more bed days than persons 18 to 44 (9.0 vs 6.2). Persons in the 65-year and older age group have the highest average bed days lost per worker due to spine pain or problems (14.9) however, a smaller proportion (11.8%) of this already small workforce reported having bed days from spine pain. Non-Hispanic white and non-Hispanic black persons recorded more bed days due to spine pain or problems (8.2; 8.7) than Hispanic persons (6.3). Comparing geographic regions, patients in the Midwest report the most bed days for spine pain (10.1), more than all other regions. (Reference Table 2A.13.1 PDF [103] CSV [104]; Table 2A.13.2 PDF [107] CSV [108]; Table 2A.13.3 PDF [109] CSV [110]; and Table 2A.13.4 PDF [111] CSV [112])
In total, 52.2 million adults in the US workforce spent more than 182 million days in bed in 2015 because of back pain, and during the same time period, almost 264 million work days were lost. The corresponding numbers of days in bed and work days lost in 2012 were 171 million and 291 million, respectively. Approximately one-third of the total workforce (31.9%) reported bed or lost work days due to back pain, but accounted for more than half of total bed days (54%0 and nearly half of total lost work days (47%). The 111.4 million workers not reporting back pain as the cause had 152.9 million bed days and 299.5 million lost work days in 2015. (Reference Table 2A.13.1 PDF [103] CSV [104])
While nonsurgical treatment for back pain is the treatment of choice, spine surgery becomes an option when neck and low back pain is disabling and not responding to nonoperative treatment alternatives. Further, in some cases such as certain fractures, infections, tumors, and severe neurologic deficits, surgery is the first treatment choice. As mentioned in earlier sections, the information we have with respect to surgical procedures is limited to that obtained from hospitals using the Nationwide Inpatient Sample. Unfortunately, the information is procedure-related and only indirectly patient-related.
In 2007, just under 1.2 million procedures for the eight most common spine procedures were performed on 662,400 patients in hospitals. In 2011, the number of patients had increased to 741,700 with a corresponding increase in the number of hospital procedures to 1.4 million. In 2013, the number of patients receiving the most common procedures, which added epidural injections to the earlier list of eight procedures, decreased to 692,585, while total procedures decreased slightly to 1.3 million. (Reference Table 2A.15 PDF [119] CSV [120])
The number of spinal decompression procedures performed, along with other procedures for which inpatient hospitalization is not always required, may not be reflected accurately because an increasing number of these patients are operated on in outpatient surgicenters and facilities. This can be, in part, illustrated here. In 2011, there were 369,900 diskectomies performed compared with 316,700 in 2013. Spinal fusion procedures were listed as the main hospital procedure, being performed 457,500 times in 2011 and 434,500 times in 2013. The majority of insertions of spinal devices, the third most common procedure group, likely occurred in patients with spinal fusions. Spinal decompression, which may or may not be performed in conjunction with a spinal fusion or in conjunction with a diskectomy, accounted for 12.5% of all procedures in 2011 and 11.8% in 2013. Changes in procedure codes for decompression between 2011 and 2013 may have partly been the cause of fewer reported decompression procedures. (Reference Table 2A.15 PDF [119] CSV [120])
Compared to the inpatient hospital setting, other healthcare sites offer a limited variety of spinal procedures. In the emergency department (ED) setting, epidural injections accounted for over 6,000 procedures, more than half of the 12,000 total procedures reported in the ED. The only procedures recorded in physician office visits were epidural injections, but they accounted for the majority of epidural injections in 2013 and reflect the variety of healthcare sites in which epidural injections can be administered. (Reference Table 2A.14 PDF [123] CSV [124])
The rate of spinal fusion procedures has risen rapidly over the past several decades. Spinal fusion is performed either alone or in conjunction with decompression and/or reduction of a spinal deformity. Fusions are performed on all regions of the spine. Lumbar fusion rates and cervical fusion rates are both increasing rapidly, while thoracic fusions continue to be less frequent. Lumbar fusions remain the most common, constituting 52% of all spine fusion procedures in 2013. Spinal refusion occurs most often to the lumbar region, accounting for 65% of both refusion procedures and refusion patients. (Reference Table 2A.16.1 PDF [127] CSV [128])
Between the years 1998 and 2013, the number of spinal fusion procedures more than doubled, from 220,000 in 1998 to 445,000 in 2013. This is a 137% increase in procedures over a 16-year period. The period from 2004 to 2011 reflected an increase of 61%, but from 2011-2013 there was a 15% decrease in recorded spinal fusions performed, most likely due to a larger proportion of these procedures being performed at an outpatient site. The rate of adult patients undergoing spinal fusion has increased from 110 per 100,000 persons in 1998 to 183 per 100,000 in 2013. During the same time period, refusion rates increased by 187% and from 6 to 13 persons per 100,000. Between 1998 and 2013, the average age of patients undergoing a fusion procedure has increased from 49.0 years to 56.4 years. (Reference Table 2A.16.2 PDF [131] CSV [132])
Although the mean length of stay for spinal fusion has decreased from 4.7 days in 1998 to 3.9 days in 2013, the mean hospital charge for these patients has increased significantly. The mean hospital charge in 1998 was $26,000 ($37,200 in 2013 dollars); while in 2013 the mean charge was $112,000. Increased use of instrumentation and biologicals (mainly bone substitutions) contribute to the higher cost. The total increase in hospital charges rose from $5.4 billion ($7.6 billion in 2013 dollars) to $48.7 billion over this 16-year period, an increase of more than 542%. Spinal refusion procedures are even more expensive, with an average charge of $129,000 in 2013, while the length of stay remained relatively constant. This, of course, does not mean that cost or reimbursement was even close to these dollar numbers. These charges are based on what hospitals set as their charges, and do not reflect the contractual agreements they have with the payer community. (Reference Table 2A.16.2 PDF [131] CSV [132])
Likely explanations for the increase in spinal fusions include advances in technology, such as the development of new diagnostic techniques and new implant devices that allow for better surgical management. In addition, there has been increased training in spinal surgery and the population has aged, presenting an increase in age-related medical problems. Further, higher expectations regarding quality of life makes patients less accepting of an ongoing back problem and more likely to look for a surgical solution.
Using the Nationwide Inpatient Sample in 2013, a broad estimate can be made of fusion procedures as it relates to admissions. In 2013, 14.6% of patients discharged with a diagnoses of back pain had a spinal fusion procedure. Males (15.4% of back pain discharges) and females (13.9%) are almost equally likely to have a fusion. Patients in the 45- to 64-year age group were slightly more likely to have a fusion procedure (19.2%) than those in the 18- to 44- years age group (15%), or in the 65- years and older age group (10.5%). Patients younger than age 18, at 24.2%, were most likely to undergo a fusion procedure when hospitalized with a diagnosis of back pain, but they constitute a very small group of patients (1.6%) among those discharged with a diagnoses of back pain. Non-Hispanic white patients hospitalized with back pain were most likely to receive a fusion (15%) when compared to non-Hispanic black (12%) and Hispanic (13%) patients. Patients in the southern United States were most likely to undergo a fusion procedure (15.7%). Patients in the western United States were second most likely to receive a spinal fusion, followed by patients in the Northeast (13.8%) and Midwest (13.3%). The length of stay was shorter if a fusion was performed than if no fusion was performed (3.9 days vs. 4.8 days), but the mean charges were more than doubled for a back pain diagnosis when a fusion was performed ($52,630 vs $110,960). (Reference Table 2A.17 PDF [137] CSV [138])
Information on the top twenty primary diagnoses and accumulative first five diagnoses for spinal fusion procedures performed in 2013 illustrates the procedure is most frequently performed in patients with lumbar spinal stenosis with or without neurogenic claudication. Lumbar disc degeneration or cervical disc displacement account for 9.6% and 9.5% of fusion procedures, respectively. (Reference Table 2A.18 PDF [141] CSV [142])
Diskectomy procedures, a surgical procedure to remove the damaged portion of a herniated disk, occurred in approximately 317,000 hosptial inpatients in 2013, with slightly more females than males undergoing the procedure. This number is likely misleading because many diskectomy procedures now occur in an outpatient setting. Of those undergoing the procedures, 35.3% had a diagnosis of either lumbar or cervical disc displacement, while 12% had a diagnosis of either lumbar or cervical disk degeneration. Approximately half of all diskectomy procedures were performed on persons in the 45 to 64 years age group, with an average age of 55.3 years. Across ethnic groups, the average age of presentation when undergoing diskectomy procedure was in the mid-50s. Non-Hispanic white patients accounted for 76% of total discharges, followed by non-Hispanic black (7.7%) and Hispanic (5.8%) patients. When comparing geographic regions, a discrepancy in charges per diskectomy was observed. The South region of the US reported the highest number of total discharges, roughly 41% of all diskectomy procedure discharges, bu this is non-unexpected given the larger share and older age of the population in the South. The Midwest ranked second in total discharges with 21%, followed by the West (20%) and Northeast (17%). (Reference Table 2A.19 PDF [145] CSV [146] and Table 2A.20 PDF [147] CSV [148])
Patients spent, on average, 3.0 days in the hospital for diskectomy procedures, a surprising number given the recent trends in discharge the same day. Although accounting for a very small number of procedures, persons younger than age 18 years had an average length of stay of 6.8 days. The mean charge for these procedures in 2013 dollars was $87,280. The western United States reported the highest charges, averaging $116,000 per procedure. This is significantly higher than the rest of the country, with the South at an averaged of just below $88,000, while the Northeast and Midwest regions were approximately $72,000. Hispanic patients averaged the highest mean charges for diskectomy procedures, estimated at $110,180. This is in comparison with a $92,730 mean charge for non-Hispanic black patients and a $86,740 mean charge for non-Hispanic white patients. (Reference Table 2A.19 PDF [145] CSV [146])
Table 2A.21 shows the diskectomy procedure trend in the United States from 1996 to 2013. It may seem surprising that the number is fairly stable given the population increase and the change in aging of the population. This is a reflection of the fact that more and more of these procedures are done in the outpatient setting and therefore not captured by the inpatient National Hospital Discharge Survey. (Reference Table 2A.21 PDF [151] CSV [152])
Persons aged 45-64 years self-report the presence of back and neck pain during a previous 3-month period in the highest numbers, at almost 27.9 million cases. Although a smaller number due to the smaller population cohort, when comparing the prevalence of all back pain, age groups 45-64 years and 65 years and older are almost identical, roughly 39% of each age group. (Reference Table 2A.1 PDF [5] CSV [6])
Healthcare visits for back disorders to doctors, emergency departments, outpatient clinics, and hospital discharges show a steady rise as the population ages up to 64 years. After that, it drops slightly. Older persons with back pain disorder are more likely to be hospitalized than are younger persons, and to stay an average of 0.5 days longer than younger persons aged 18 to 64 years. Average charges for hospital stays with a diagnosis of back pain also increase with age. While the prevalence of neck disorders is significantly lower, aging also has a large impact on the number of healthcare visits for neck pain. (Reference Table 2A.2.2 PDF [23] CSV [24] and Table 2A.10.2 PDF [41] CSV [42])
Limitations of daily living due to chronic back pain increase in prevalence as the population ages. Back pain is listed as a cause of limitations by 6.4% of persons 65 and older, compared to 2.7% of the total population. Back pain represents the cause of limitations for roughly 1 in 5 persons with limitations due to any cause for both all persons and those age 65 and older (19.7% and 19.2%, respectively). (Reference Table 2A.11.2 PDF [95] CSV [96])
Back pain is a major health concern to older people. As the population ages, back pain becomes an increasing burden on the healthcare system.
Economic burden in The Burden of Musculoskeletal Diseases (BMUS) is based on data from the AHRQ Medical Expenditure Panel Survey (MEPS). The MEPS, which began in 1996, is a set of large-scale surveys of families and individuals, their medical providers (doctors, hospitals, pharmacies, etc.), and employers across the United States. MEPS collects data on the specific health services that Americans use, how frequently they use them, the cost of these services, and how they are paid for, as well as data on the cost, scope, and breadth of health insurance held by and available to US workers. Data reported in BMUS is based on three-year averages for each sequence of years.
Between the years 1996 to 1998 and 2012 to 2014, the number of persons in the population reporting a spine condition rose from 27.4 million to 34.9 million, but the proportion of total population with a spine condition (10.1% vs 11.0%) increased only slightly over the nearly two decades. However, distribution of the population with a spine condition, by age group, showed a consistent shift upward as the population ages, reflecting the overall aging of the US population. (Reference Table 8.12 PDF [155] CSV [156])
Healthcare treatments and visits contribute to the burden of spine conditions. Ambulatory physician visits, home health care visits, and hospital discharges all rose by 34%, 46%, and 28%, respectively, between the years 1996 to 1998 and 2012 to 2014. Mean visits for these three healthcare providers and share of spine patients using them remained relatively steady, indicating the primary reason for the increase is population growth. While still accounting for a relatively small number of visits, ambulatory non-physician care visits rose from 101 million in the earlier time frame to 220 million in the most recent years, an increase of 117%, due to both an increase of spine patients using this resource and a jump in mean visits.
However, prescription medications for spine conditions show the most dramatic rise, jumping from 353 million prescription fills to 789 million between the time frames, an average increase per year of 7.3% with a total increase of 123%. This increase was due primarily to the increase in mean number of refills per person, from 12.0 to 22.6, rather than the share of persons with a spine condition obtaining prescriptions, an increased share of only 3.5%. (Reference Table 8.2.2 PDF [159] CSV [160])
Overall, ambulatory care visits (physician office visits, non-physician visits, and home health care visits) accounted for the largest share of per person direct cost for persons with a spine condition. At an average cost of $3,220 per person between 2012 and 2014, an increase of 82% from 1996 to 1998 in 2014 dollars, ambulatory care accounted for 36% of per person direct cost between 2012 and 2014. While the share of mean per person cost for inpatient care dropped from 36% to 25% between 1996 and 1998 and 2012 and 2014, the mean cost rose from $1,823 to $2,258 in 2014 dollars, an increase of 24%. At the same time, the average per person cost for prescriptions rose from $675 to $2,263, in 2014 dollars, an increase of 235%. (Reference Table 8.4.2 PDF [163] CSV [164])
Total direct per person healthcare costs for persons with a spine condition were $9,035, an increase of 80% since 1996 to 1998 based on 2014 dollars. Incremental direct per person costs, those costs most likely attributable to a spine condition, rose from $970 to $1,615, in 2014 dollars, an increase of 66%. (Reference Table 8.6.2 PDF [13] CSV [14])
Total aggregate direct costs for all persons with a spine condition were $315.4 billion in 2012 to 2014, a rise of 129% from the $13 billion in 1996 to 1998, in 2014 dollars. Incremental aggregate direct costs increased from $26.6 billion in 1996 to 1998 to $56.4 billion in 2012 to 2014, an increase of 112%. (Reference Table 8.6.2 PDF [13] CSV [14])
Indirect costs associated with lost wages for persons ages 18 to 64 years are not calculated for persons with a spine condition. However, back pain is often cited as the reason for bed days and lost work days by persons in the labor force. In 2015, 4.9 million persons in the prime working ages of 18 to 64 years reported they are unable or limited in work at the time due to chronic back or neck problems. (Reference Table 2A.11.2 PDF [95] CSV [96])
Also, in 2015, 14.3% of the workforce age population reported an average of 7.8 bed days in the previous 12 months, for a total of 182 million bed days, due to chronic back or neck pain. In addition, 15.4% of this same population reported an average of 10.5 lost work days in the previous year due to chronic back or neck pain, or approximately 264 million work days lost due to back pain. (Reference Table 2A.13.1 PDF [103] CSV [104])
The financial cost associated with back pain is obviously enormous and, unfortunately, rising. At the current rate of increase, back pain treatment will quickly become unsustainable. Greater understanding of the underlying causes of back pain, ability to sub-classify patients based on accurate pain generators (eg, discogenic pain, facet mediated pain, radicular pain) and what factors lead to disability (ie, biological, psychological, or social) is needed to reduce this continually increasing trend. Ideally, understanding the variability of individual sources of and contributions to back pain could direct clinicians to specific treatments that best address the diagnosis.
The cost and difficulty of back pain research is also a major challenge. The complexity of back pain diagnosis and treatment options make high quality clinical research with meaningful results very difficult to fund and complete. This requires large scale multi-center trials with well-educated research staff and patients willing to stick with randomized modes of treatment. The latter consideration is often very difficult to obtain in a system where patients want immediate results. In addition, many non-surgical, non-pharmacological providers use a multimodal approach to care rather than an isolated intervention, complicating efforts to identify which treatment is most effective.
Adding to this challenge may be the subjective nature of pain. It is often very difficult, if not impossible, to separate psychological or emotional pain that is greatly influenced by the social environment from physiologic pain caused by a specific physical source. Differentiating between the two categories will play a tremendous role in our ability to treat patients in pain. Societal perceptions about back pain have been shown to lead to catastrophization, a common cognitive distortion extensively studied in psychology that is an irrational thought or belief that something is far worse than it actually is. Studies in pain patients have found catastrophization to be a significant factor in their disability and response to treatment.
System integration of historically fringe practitioners is a challenge as we attempt to grow effective non-surgical management strategies such as acupuncture, massage, tai chi, yoga, and chiropractic. Training practitioners to provide evidence-based informed care plans and appropriate referrals for other services or emergent conditions should start early in medical training. Improved graduate and post-graduate education which includes integrating educational tracks to better understand different disciplines of care and what they can offer can create a shared common base of critical thinking. For example, Denmark provides the first year medical school education to chiropractors and physicians jointly before diverging to more specific training.
Another challenge to the future is our healthcare financial system. Treatment decisions are too often made based on financial limitation rather than best clinical practice. Clinical decisions may be limited by insurance authorizations or treatment decisions, and could be influenced by highest reimbursement. Cost-effectiveness and risk/benefit discussions for alternative options are essential to providing successful treatments and reducing costs.
Understanding why the degenerative cascade causes pain in some, yet not in others, is needed to address the burden of pain and disability and the significant economic impact low back pain treatments create on healthcare resources each year.
One of the greatest unmet needs related to back pain is the ability to clearly diagnose the source of back pain. There are so many physical and non-physical sources of back pain that patients are often treated inappropriately before they are clearly diagnosed. Thousands of dollars are often spent on diagnostic evaluations without finding a clear source of back pain, a process that needs to be broken by earlier diagnosis, earlier definitive treatment, and maintenance of the ability to continue working.
Most patients with back and neck pain are treated non-operatively, often with alternative treatments, including such treatments as acupuncture, homeopathy, and massage. We know that enormous amounts of money are spent on many of these treatments, yet no quantifiable measures of cost or effect are yet available. Furthermore, the lack of information about treatments by chiropractors, physical therapists, and other care providers results in underestimated cost estimates for treatment of low back pain. There is also a lack of information on medical procedures done in offices or surgicenters, limiting estimates of cost and effectiveness of many interventional procedures, including many surgical procedures. These gaps in knowledge should be filled to obtain accurate estimates of the impact of back and neck pain on society.
As such, there remains debate regarding the most effective treatment for low back pain. Increased recommended alternatives to non-surgical options adds credence for improved informed consent, creating conversation about benefits and risks and leading to a better shared decision making process for the patient. Though research is limited, per Zaina et al, informing the patient of anticipated outcomes of not only surgery but other options is vital. In a systematic review performed by Zaina et al, the authors evaluated the effectiveness of different types of surgery compared with different types of non-surgical intervention in the treatment of low back pain secondary to lumbar spinal stenosis (LSS).1 The authors’ analysis demonstrated no differences in pain-related disability improvement between surgical (decompression with or without fusion) and non-surgical care. However, due to the low quality of available studies, the authors were unable to confidently recommend a preferable treatment method for symptomatic LSS.
To begin addressing these needs, there has been an increase in research on the efficacy of non-surgical interventions for low back pain. Ammendolia et al investigated the safety and effectiveness of epidural injections to other treatments for symptomatic LSS.2 Due to the low overall evidence (only 4 randomized controlled trials), the authors were only able to conclude that epidural injections provide improved pain, function, and quality of life for only up to 2 weeks.
Another area of increased interest is the effect of pre- and postoperative spinopelvic parameters (the relationship of the pelvic position to the spine) on treatment outcomes. Several previous investigations have described the magnitude of parameter correction afforded by surgical and non-surgical treatment modalities. However, many of these studies have featured small sample sizes and have rarely offered level I or II evidence. As such, there exists a need for large, prospective studies that investigate the true impact of influence of spinopelvic parameters on treatment outcomes for low back pain.
Acupuncture has been utilized in the treatment of low back pain for centuries, and has recently been established as a non-operative complimentary treatment in the United States.3 A meta-analysis evaluating the use of acupuncture in the treatment of low back pain demonstrated the use of acupuncture as a complimentary, highly cost-effective treatment.4 According to the World Health Organization (WHO) cost-effectiveness threshold values, the cost of complimentary acupuncture treatment was determined to be $48,562 per disability-adjusted life year (DALY) avoided. Interestingly, in patients where comorbid depression was also alleviated at the same rate as pain, the cost was revealed to be $18,960 per DALY avoided. The authors concluded that acupuncture, as a substitute for standard care, was most cost-effective when used in patients with comorbid depression.
As noted in the previous discussion of Indirect Costs [171], back pain was the cause of close to 264 million lost work days in a 12-month period during 2014-2015. In addition, over 4%, or 1 in 25, persons in the prime working ages of 18 to 64 report they are either limited in the type or amount of work they can do or are unable to work at all due to back pain. It is clear that back pain has a substantial impact on the workforce, and that finding ways to reduce or repair causes of back pain is needed. (Reference Table 2A.11.2 PDF [11] CSV [12])
In general, there is a need for high quality clinical research in treatment of low back pain. This includes addressing the lack of evidence for best practices for non-surgical active care approaches and surgical treatment. Additionally, work-related back pain has the potential to become "chronic" back pain, often with co-morbid dependence on narcotic pain medications. This process needs to be broken by earlier diagnosis, maintenance of ability to continue working, and earlier definitive treatment.
There is a need to promote a culture of "stopping back pain before it starts" by adopting spine care procedures, such as proper posture and balance exercise regimes, by persons of all ages as a counter to back pain. In addition to BMUS, the World Spine Care and Global Spine Care Initiative are coalitions all working to find ways to reduce back pain and back pain costs.
Back Pain (Lumbar and Low Back):
Back Disorders:
Ankylosing spondylitis and other inflammatory spondylopathies: 720*
Spondylosis and allied disorders: 721.2-721.9
Other and unspecified disorders of back: 724
Disk Disorders:
Displacement of intervetebral disc: 722.10, 722.11
Schmorl's nodes: 722.30-722.39
Degeneration of intervetebral disc: 722.51, 722.52, 722.60
Intervertebral disc disorder with myelopathy: 722.72, 722.73
Postlaminectomy syndrome: 722.80, 722.82, 722.83
Other and unspecified disc disorder: 722.90, 722.92, 722.93
Back Injury:
Closed fracture of vertebra without mention of spinal cord injury: 805.20-805.80
Closed fracture of vertebra with spinal cord injury: 806.20-806.90
Closed dislocation, vertebra: 839.20-839.49
Sprains and strains of sacroiliac region: 846
Other sprains and strains of back: 847.10-749.90
Cervical (Neck) Pain:
Neck Disorders:
Cervical spondylosis: 721.00, 721.11
Disorders of cervical region: 723.00-723.90
Disk Disorders:
Displacement of cervical intervertebral disc: 722.00
Degeneration of cervical intervertebral disc: 722.40
Intervertebral disc disorder, with myelopathy: 722.71
Postlaminectomy syndrome of cervical region: 722.81
Other and unspecified disc disorders of cervical region: 722.91
Neck Injury:
Closed fracture of cervical vertebra without mention of spinal cord injury: 805
Closed fracture of cervical vertebra with spinal cord injury: 806
Closed dislocation, cervical vertebra: 839
Neck sprain: 847.00
Spine Procedures (ICD-9-CM Procedures Code)
Cervical fusion: 81.02, 81.03
Thoracic fusion: 81.04, 81.05
Lumbar fusion: 81.06-81.08
Other fusion: 81.00, 81.01
Fusion/refusion multiple vertebrae: 81.62-81.64
Spine refusion: 81.30-81.39
Spinal decompression: 03.09
Spinal diskectomy: 80.50, 80.51
ICD-9-CM to ICD-10-CM CODE CONVERSION
Direct conversions between the ICD-9-CM codes used in this analysis to ICD-10-CM codes is difficult due to the greatly expanded diagnosis codes in ICD-10-CM. For example, converting the six codes included in the Lumbar/Low Back Back Disorders group returns only six general or unspecified codes related to the spondylopathies whereas, in reality, there are five major classifications (M45, M46, M47, M48, M49) each of which is broken down into specific conditions that are further broken down by site. For example, using only the M45 and M46 codes (shown below) there are 80 new codes.
M45 Ankylosing spondylitis
M45.0 Ankylosing spondylitis of multiple sites in spine
M45.1 Ankylosing spondylitis of occipito-atlanto-axial region
M45.2 Ankylosing spondylitis of cervical region
M45.3 Ankylosing spondylitis of cervicothoracic region
M45.4 Ankylosing spondylitis of thoracic region
M45.5 Ankylosing spondylitis of thoracolumbar region
M45.6 Ankylosing spondylitis lumbar region
M45.7 Ankylosing spondylitis of lumbosacral region
M45.8 Ankylosing spondylitis sacral and sacrococcygeal region
M45.9 Ankylosing spondylitis of unspecified sites in spine
M46 Other inflammatory spondylopathies
M46.0 Spinal enthesopathy
M46.00 …… site unspecified
M46.01 …… occipito-atlanto-axial region
M46.02 …… cervical region
M46.03 …… cervicothoracic region
M46.04 …… thoracic region
M46.05 …… thoracolumbar region
M46.06 …… lumbar region
M46.07 …… lumbosacral region
M46.08 …… sacral and sacrococcygeal region
M46.09 …… multiple sites in spine
M46.1 Sacroiliitis, not elsewhere classified
M46.2 Osteomyelitis of vertebra
M46.20 …… site unspecified
M46.21 …… occipito-atlanto-axial region
M46.22 …… cervical region
M46.23 …… cervicothoracic region
M46.24 …… thoracic region
M46.25 …… thoracolumbar region
M46.26 …… lumbar region
M46.27 …… lumbosacral region
M46.28 …… sacral and sacrococcygeal region
M46.3 Infection of intervertebral disc (pyogenic)
M46.30 …… site unspecified
M46.31 …… occipito-atlanto-axial region
M46.32 …… cervical region
M46.33 …… cervicothoracic region
M46.34 …… thoracic region
M46.35 …… thoracolumbar region
M46.36 …… lumbar region
M46.37 …… lumbosacral region
M46.38 …… sacral and sacrococcygeal region
M46.39 …… multiple sites in spine
M46.4 Discitis, unspecified
M46.40 …… site unspecified
M46.41 …… occipito-atlanto-axial region
M46.42 …… cervical region
M46.43 …… cervicothoracic region
M46.44 …… thoracic region
M46.45 …… thoracolumbar region
M46.46 …… lumbar region
M46.47 …… lumbosacral region
M46.48 …… sacral and sacrococcygeal region
M46.49 …… multiple sites in spine
M46.5 Other infective spondylopathies
M46.50 …… site unspecified
M46.51 …… occipito-atlanto-axial region
M46.52 …… cervical region
M46.53 …… cervicothoracic region
M46.54 …… thoracic region
M46.55 …… thoracolumbar region
M46.56 …… lumbar region
M46.57 …… lumbosacral region
M46.58 …… sacral and sacrococcygeal region
M46.59 …… multiple sites in spine
M46.8 Other specified inflammatory spondylopathies
M46.80 …… site unspecified
M46.81 …… occipito-atlanto-axial region
M46.82 …… cervical region
M46.83 …… cervicothoracic region
M46.84 …… thoracic region
M46.85 …… thoracolumbar region
M46.86 …… lumbar region
M46.87 …… lumbosacral region
M46.88 …… sacral and sacrococcygeal region
M46.89 …… multiple sites in spine
M46.9 Unspecified inflammatory spondylopathy
M46.90 …… site unspecified
M46.91 …… occipito-atlanto-axial region
M46.92 …… cervical region
M46.93 …… cervicothoracic region
M46.94 …… thoracic region
M46.95 …… thoracolumbar region
M46.96 …… lumbar region
M46.97 …… lumbosacral region
M46.98 …… sacral and sacrococcygeal region
M46.99 …… multiple sites in spine
and so on. Future analysis for BMUS will require identification of new categories for analysis of spine low back and neck diagnoses.
Conversion of the spine procedure codes was made and can be viewed by clicking HERE [172]. Again, the number of codes is greatly expanded, with more than 650 new codes representing the 25 spine procedure codes analyzed in this Fourth Edition of The Burden Of Musculoskeletal Diseases in the United States.
A normal spine is structurally balanced for optimal flexibility and has gentle front-to-back inward and outward curves that work in harmony to keep the body’s center of gravity aligned over the hips and pelvis. The cervical spine (neck) and lumbar (lower) spine both have a lordosis, an inward or concave curve, while the thoracic (middle) spine has a kyphosis, an outward or convex curve. Together these curves form a gentle S.
Spinal deformity is caused by abnormal curvature of the spine putting it out of alignment. When the abnormal curvature is seen from the side (a front-to-back imbalance) it is called sagittal imbalance, and includes the conditions of kyphosis, lordosis, and spondylolisthesis resulting in flatback syndrome and chin-on-chest or dropped head syndrome. When seen from the back (a side-to-side imbalance) it is called scoliosis. While scoliosis can be caused by conditions such as cerebral palsy, muscular dystrophy, and a broad spectrum of conditions (acquired or secondary scoliosis), the cause of most scoliosis is unknown (idiopathic scoliosis). Spinal deformity affects individuals in every age and demographic group, but the prevalence increases with age as many causes are affected by degenerative conditions.
Spinal deformity has a significant and measurable impact on health-related quality of life, including pain, function, self-image, mental health, work status, and disability. Prevalence of disease, utilization of healthcare resources, impact of disease on health-related quality of life, and cost of care are useful tools for measuring the burden of deformity on our population and on our healthcare economy. The purpose of this chapter is to provide information on the burden of spinal deformity on patients and on our healthcare system.
Adult spinal deformity is a broad diagnostic classification that includes idiopathic scoliosis as well as de novo or degenerative curves, which often result in coronal and/or sagittal plane decompensation. Sagittal plane malalignment is an increasingly recognized cause of pain and disability.1
The prevalence of spinal deformity has been reported at a wide range depending on the type of deformity and age. Congenital scoliosis has been reported at 100 in 100,000 persons,2 with acquired deformity as high as 68,000 in 100,000 persons.3 (Reference Table 2B.1.0 PDF [173] CSV [174])
Conditions related to the spine and spinal deformity often sound similar but affect the spine in different ways. Key conditions discussed in this section include the following.
Curvature of the spine: Spine curvature can refer to two distinct conditions. The human spine normally curves, but more commonly the term "spinal curvature" refers to abnormalities from the standard spinal.
• Idiopathic: Of unknown cause. Any disease that is of uncertain or unknown origin may be termed idiopathic; usually associated with children who develop an abnormal curvature at a young age.
• Acquired: Curvature that develops over many years, usually associated with adults and older persons.
• Secondary: Curvature caused by another condition, such as osteoporosis.
Sagittal imbalance: Deformity where loss of the normal lordosis of the lumbar spine or increased kyphosis of the thoracic and thoracolumbar spine causes the torso and head to pitch forward relative to the hips and pelvis. Loss of lordosis in the lumbar spine is also known as flat back syndrome.
Scoliosis: Side-to-side abnormal curvature of the spine.
Spondylolisthesis: Forward movement of one vertebra in relationship to a vertebra below it.
Spondylosis: Degeneration of the disc spaces between the vertebrae. Spondylosis is common with aging and affects virtually everyone to some degree after the age of 60 years. When severe, it can cause local pain and decreased range of spinal motion, requiring pain and/or anti-inflammatory medications.
Stenosis: A narrowing of the open spaces within the spine, which can put pressure on the spinal cord and the nerves that travel through the spine. Spinal stenosis occurs most often in the neck and lower back.
Kyphosis: An abnormal, convex curvature of the spine, with a resultant bulge at the upper, middle or lower back.
Spinal fractures:
• Traumatic spine fractures (TF): High-energy fractures resulting from accidents, falls, and sports.
• Vertebral compression fractures (VCF): Low-energy fractures in the aging as a result of reduced bone density and strength (osteoporosis and osteopenia).
Spinal infection:
• Tuberculosis of spine: An infection that usually occurs in the lungs, but can also occur in the spine, resulting in destruction of the intervertebral disk space and adjacent vertebral bodies. It is more common in children and young adults.
• Intraspinal abscess: A collection of pus and infectious material in the spine.
• Osteomylitis: A bone infection normally caused by bacteria but sometimes by fungus. The infection can occur in any bone but typically affects the arms, legs, spine, and pelvis. The bacteria usually reach the bone from an injury or wound. It can be either acute, where symptoms of pain, swelling, and fever last only a few months, or chronic.
• Discitis: Infection exists in the small spaces between these bones (the intervertebral disc spaces), which puts pressure on the discs and causes pain. Discitis is relatively uncommon and mostly affects young children.
• Postoperative infections: Infections after surgical procedures (operations) can cause pain, poor wound healing, need for further treatment including antibiotics, longer hospital stays, and increased healthcare costs.
Complications of surgery: Common surgery complications, including excessive blood loss, pain, infection, neural injury, anesthesia effects, blood clots, and other medical complications (heart attack, stroke).
Spondylopathies: Any disease of the vertebrae or of the spinal column.
Surgical procedures: Often performed to reduce pain and deformity from spinal curvature including osteotomies ( complete or partial removal of the vertebral bodies), spinal instrumentation, and fusion.
• Spinal fusion: A surgical procedure in which two or more vertebrae are permanently joined into one solid bone with no space between them.
• Osteotomies: A surgical procedure in which a portion of the vertebral body is removed to help restore the normal alignment of the spine. The procedure is utilized to reduce the amount of kyphosis or increase lordosis.
The normal spine viewed from the side forms a gentle "S" shape. When viewed from the back, the normal spine appears straight. The naturally occurring soft curves of the spine are designed to distribute mechanical stress in the body when at rest and during movement. When the curvature is even slightly abnormal, a person may experience occasional mild or annoying discomfort. If the curve is severely abnormal, the pain is usually severe and accompanied by disability. Scoliosis occurs in both children, where it is generally idiopathic, and adults, where it is often acquired.
In 2013, there were nearly 2 million healthcare visits with a diagnosis of scoliosis, the majority of which 1.3 million were to a physician’s office. However, 166,600 hospital discharges had a scoliosis diagnosis. The number of hospital discharges with a scoliosis diagnosis has remained relatively steady for five years (2010 thru 2014) and represents approximately 56 persons in every 100,000 US population. Females accounted for three out of four (73%) of healthcare visits with a scoliosis diagnosis. (Reference Table 2B.2.0 PDF [175] CSV [176] and Table 2B.2.1 PDF [177] CSV [178])
Spinal deformity and scoliosis can be found at birth due to genetic causes, develop during childhood, or occur late in life because of degenerative disc and joint disease. Common signs of scoliosis are a prominent shoulder or shoulder blade, or chest wall asymmetry. Another sign is uneven hips, with one hip seemingly higher than the other hip. It is important not to confuse scoliosis with poor posture and to realize that scoliosis will usually not disappear with age. Despite the severity of these conditions and the impact they have on the lives of children, the prevalence of spinal deformities in children under the age of 18 years is difficult to determine because of relatively low numbers and the degree to which the condition manifests initially in pain or disability. Estimated prevalence of spinal deformity conditions has been cited in numerous studies, and ranges from 0.4 in 1,000 for infantile idiopathic scoliosis1 to 2.5 in 1,000 for adolescent idiopathic scoliosis.2 (Reference Table 2B.1.0 PDF [173] CSV [174])
There are several different types of scoliosis. The most common type of scoliosis is idiopathic, meaning the cause is unknown. Approximately 80% to 85% of scoliosis cases are idiopathic.3 Idiopathic scoliosis can occur as early as the first three years of life, which is known as infantile idiopathic scoliosis. If diagnosed between the ages of 4 to 10 years, it is known as juvenile idiopathic scoliosis, and from 10 years of age to skeletal maturity, as adolescent idiopathic scoliosis. The term “early onset scoliosis” (EOS) is also used to describe scoliosis that occurs prior to 10 years of age. Adolescent idiopathic scoliosis is the most common type.
Scoliosis, if severe enough (>25°), is usually treated with bracing if the child is growing or with surgery if the curvature is more severe (>45° to 50°). The standard radiograph measurement method for all forms of scoliosis is the Cobb angle measurement technique, measured from the end plates of the maximally tilted end vertebral bodies in a standing radiograph.4 Whether the curve is >25° or >40° to 45°, the treatment is preventative in nature, helping to avoid progression of the curve and more significant future problems that might occur if it was left untreated. Increased mortality has been reported in untreated early onset scoliosis due to respiratory conditions.5 While this preventative aspect is hugely valuable and intuitively important, its benefit is difficult to measure from a public health standpoint, especially for rare conditions of childhood such as juvenile and adolescent pediatric scoliosis.
Infantile scoliosis occurs in patients 0-3 years old and currently accounts for less than 1% of all cases of idiopathic scoliosis in the United States. Boys are affected by infantile idiopathic scoliosis at a higher rate than girls (3:2 ratio).1 Infantile scoliosis curves tend to be left-sided (75% to 90%). Past studies have indicated this rare type of scoliosis occurs more frequently in Europe than in North America.6
Treatment for patients with infantile idiopathic scoliosis is determined by anticipated or actual curve progression. Several common measurement techniques are used, with angles ≤20° generally considered at low risk for progression. In addition to measuring the Cobb angle, the rib-vertebra angle difference (RVAD) is used as a common predictor of curve progression.7 Patients with a Cobb angle of ≤25° and a RVAD of ≤20° are at a low risk for progression and should be re-evaluated every 4 to 6 months.1
Nonsurgical treatment, such as bracing or casting, is initiated if a curve progression of ≥10° occurs. Surgical treatment should be considered when nonsurgical measures, including both bracing and casting, are not successful. Surgical treatment is utilized when a curve is ≥45° and progressive in an immature child.1 Overall, surgical methods are continually evolving, with the goal of obtaining and maintaining curve correction while simultaneously preserving or encouraging spinal and trunk growth.
Surgical options currently utilized include various types of spinal fusion or hemiepiphysiodesis, a minimally invasive implant procedure to slow progression of curve growth. Additional techniques include growing-rod instrumentation (rods that expand and support the deformed spine) and vertical expandable (telescoping) prosthetic titanium rib (VEPTR) instrumentation.8 The goal of using surgical methods is to halt the progression of the curve and gain correction of the deformity, while allowing maximum growth of the spine, lungs, and thoracic cage.1 The allowance of normal lung development is one of the critical factors in recommending treatment for infantile and juvenile idiopathic scoliosis. Prevention of early mortality due to respiratory failure is a key driver of surgical treatment of early onset scoliosis.1,5
In 12% to 21% of idiopathic scoliosis cases, the diagnosis is made between 4 and 10 years of age. Between the ages of 4 and 6 years, the female-to-male ratio of juvenile idiopathic scoliosis is 1:1. However, the ratio of female to male cases rises to between 2:1 and 4:1 in children between the ages of 4 and 10 years, and to 8:1 in children who are 10 years of age or older.9 Both right and left curves are found with equal frequency for patients younger than 6 years, but rise to a 3:1 ratio of right versus left thoracic curves after the age of 6.10
Observation is the main treatment for patients with a small curve of less than 20° to 25°. Follow-up visits are recommended every 4, 6, 9, or 12 months, depending on the patient’s age, the degree of the curve, and the characteristics of the clinical deformity.9
Curves between 25° and 50° are usually treated with bracing in this age group. Bracing can be done either on a part- time or full-time basis, depending on the size of the curve as well as the age of the child. A study completed in 1982 evaluating the success of bracing reported an excellent prognosis when part-time bracing was utilized for patients with a curve of ≤35° and RVAD11 of ≤20°; however, curves ≥45° and RVAD of ≥20° had a less favorable prognosis for successful treatment with bracing.9
Overall, the curve patterns in patients with juvenile idiopathic scoliosis are similar to those with adolescent idiopathic scoliosis. Approximately 70% of patients with juvenile idiopathic scoliosis exhibit curve progression and require some form of treatment. In a study conducted in 1981, 55 of 98 patients (56%) with juvenile idiopathic scoliosis required spinal surgery. The most common and traditional surgery is posterior instrumentation and fusion.9
According to the Scoliosis Research Society (SRS), idiopathic scoliosis is diagnosed when a patient has asymmetry on forward bending combined with a curve of at least 10°.12 By this definition, the prevalence of adolescent idiopathic scoliosis in children from 11 to 18 years of age is 2% to 3%. Though the male-to-female ratio for smaller curves is about equal, larger curves seem to be more common in females. Similar results were found in a study conducted in 1985, where 29,195 children were screened for idiopathic scoliosis.2
Several studies have investigated the natural history and natural course of curve progression in adolescent idiopathic scoliosis. All report the strongest predictive factors in the development of idiopathic scoliosis are age, magnitude of curve, and gender.13,14,15,16 Girls are more likely to have adolescent idiopathic scoliosis than boys, and some studies report the onset is earlier in girls than boys. A factor highly correlated with curve progression is age at diagnosis; patients diagnosed at a younger age have a greater risk of curve progression. However, those diagnosed at a younger age seem to have a more favorable response to milder forms of treatment, which supports the practice of school screening to detect and lead to earlier diagnosis for those children who exhibit a smaller degree of curvature.
Treatment decisions for individuals with adolescent idiopathic scoliosis are made based on location, shape, pattern, and cause of the curve. The treatment choice is also a function of the patient’s future growth potential. Treatment choices include observation, bracing, and surgery. Observation is usually reserved for patients who have curves ≤25°. Bracing, which is used to stop curve progression (rather than for lasting correction of the curve), is usually used for patients who have curves ≥25° and who are still growing. Surgery is generally used for patients with curves ≥45°.
Congenital scoliosis is believed to affect approximately one child for every 1,000 live births.17 The cause is unknown in most cases, but in some cases, it is associated with various syndromes, as shown in the illustration below. Diagnosis occasionally is made during prenatal ultrasound. In cases of congenital scoliosis, additional congenital conditions, such as chest wall malformation or kidney or heart abnormalities, are often present. Treatment options for congenital scoliosis are bracing and/or surgery and are similar to treatments discussed for idiopathic scoliosis. Bracing is not as effective for congenital scoliosis as it is for idiopathic scoliosis.
Major abnormal spinal deformity occurring during infancy or early childhood poses a clinical problem because of the anticipated long growth period (at least 10 years), variable presentation and treatment methods, and the length of time that must pass before meaningful outcome results can be assessed in the small number of patients for definitive studies. Curves that result from congenital scoliosis are often not treated as easily as idiopathic curves because the deformity is in the bones rather than the soft tissue, causing the curve to be rigid.18
Scoliosis also occurs in conjunction with several congenital conditions that occur in infancy or childhood. These include muscular dystrophy, cerebral palsy, spina bifida, and spinal muscular atrophy. Scoliosis associated with these conditions is referred to as neuromuscular scoliosis. Both the likelihood and the severity of the scoliosis generally increases with the severity of the underlying condition. For example, a child with severe cerebral palsy who is unable to walk is more likely to have severe scoliosis than a child with mild cerebral palsy who can walk.
Because of the low prevalence of scoliosis in children and adolescents, it is difficult to analyze the healthcare impact on the US healthcare system from this condition. However, the impact of scoliosis over a lifetime due to pain, inability to work, and cost to the healthcare system are substantial.
In 2013, one in three (35%) healthcare visits with a diagnosis of scoliosis was for a person under the age of 18. Most visits, 93% of the 681,100, were classified as idiopathic scoliosis. The majority (93%) of all visits with a diagnosis of scoliosis by persons under age 18 were outpatient visits to either an outpatient clinic or physician office. Only 3.5% represented hospital discharges; however, this still accounted for 23,800 discharges for this often painful condition in children and adolescents. (Reference Table 2B.2.2 PDF [190] CSV [191])
In 2013, 40% of children and adolescents under the age of 18 years discharged from the hospital with a diagnosis of scoliosis had surgery. Spinal fusion was the most common surgery performed (36.1%), followed by incision/excision (24.6%), and deformity monitoring (9.6%). One in seven (15%) also had a blood transfusion. (Reference Table 2B.5.2 PDF [194] CSV [195])
Average hospital charges for patients under 18 years of age with a scoliosis diagnosis in 2013 were five times the average charge for all hospitalized patients in this age group ($113,800 versus $22,400), even though the length of stay was only about 50% longer (6.4 days versus 3.9 days). The high number of surgical procedures likely accounted for some of this variance. The length of stay and mean charges were slightly higher for those with an acquired/secondary scoliosis diagnoses than for those with an idiopathic scoliosis diagnosis. (Reference Table 2B.3.2 PDF [198] CSV [199])
Young people under the age of 18 with scoliosis are four times more likely to be transferred to a long-term care facility and three times more likely to have home healthcare than peers discharged for any diagnosis although the rates are still lower than among older persons (3% and 9%, respectively). (Reference Table 2B.4.2 PDF [204] CSV [205])
Deformity of the adult spine includes patients with curvature of the spine (scoliosis) of varying degrees caused or impacted by degenerative disc and joint disease. Adult scoliosis may be the result of persistent or progressive deformity since adolescence or a new, de novo, onset of deformity resulting from degeneration or aging of the spine. Degenerative scoliosis accounts for most scoliosis cases in older populations aged 65 years and older, as reflected in the low proportion of older patients with a diagnosis of primary idiopathic scoliosis.
Degenerative scoliosis is one of the most challenging spine conditions to treat because of the variability of the condition. Generally, it is thought to originate with the degeneration of the intervertebral discs, which leads to misalignment of the vertebral column. Degenerative scoliosis, particularly in the very elderly, is often associated with other conditions, such as osteoporosis. Treatment outcomes for both nonsurgical and surgical procedures are not well documented; hence, recognition and earlier intervention are important to ward off the more complex problems of adult scoliosis. The role played by undiagnosed, mild idiopathic adolescent scoliosis on the development of degenerative scoliosis in later life is unknown.
The clinical presentation and management of adults with scoliosis is characterized by a great deal of variability. There is a poor correlation between the magnitude of deformity and the impact of scoliosis on health status, as patients with large spinal curvatures may have limited pain and disability and patients with relatively mild deformity may be severely impaired. Deformity in the sagittal plane is associated with disability more than scoliosis.1 Patients with adult scoliosis seek medical care for symptoms, including back pain, neural symptoms, and progression of deformity. It is often neural symptoms secondary to spinal stenosis that leads patients to seek treatment.
The prevalence of adult spinal deformity and scoliosis is not well established, with estimates ranging from 2.5% to 25% of the population.2,3,4,5,6,7 A 2005 study reported mild to severe adult scoliosis prevalence as high as 68% in a healthy (no known scoliosis or spine surgery) population aged 60 years and older.8 Many cases of degenerative scoliosis are undiagnosed, but elderly patients often seek care because of back and leg pain that may be caused by scoliosis and associated spinal stenosis.
According to 2010 US Census Population Estimate, there were 235,205,658 people in the United States over the age of 18 years. Prevalence of adult scoliosis cited in the literature ranges from 2.5% to 60%, depending on severity. A conservative estimate (2.5%) of the prevalence of adult scoliosis yields an incidence of a minimum of 5.88 million adults in the United States with adult scoliosis. In 2013, an estimated 1.28 million of these adults received treatment either as an inpatient or on an outpatient basis. (Reference Table 2B.2.2 PDF [190] CSV [191])
The management of adult scoliosis includes nonsurgical and surgical resources. Nonsurgical treatments of adult scoliosis utilize significant resources, and include interventions such as exercises, physical therapy, injections, pain medications, and manual manipulation.9 Data on nonsurgical treatments is not available; however, a 2010 nonrandomized study reported that two years of nonsurgical treatment in adult scoliosis patients resulted in substantial expenditures and yielded no improvement in health status.10
Operative management of scoliosis in the adult encompasses a spectrum of procedures, including decompression alone, decompression with limited fusion, and fusion of the deformity. The type of procedure performed is typically determined by the predominant symptoms. Neural symptoms in patients with smaller curves (<30 degrees) are treated with decompression alone, while patients with larger curves and neural symptoms are treated with decompression and fusion.11 Adult scoliosis associated with sagittal deformity is more commonly treated with decompression, osteotomies, and larger fusions of greater than four level (five or more vertebrae).12
In 2013, a query of the Healthcare Costs and Utilization Project (HCUP) Nationwide Inpatient Survey (NIS) resulted in approximately 142,600 hospitalizations of people age 18 and over associated with a discharge diagnosis of scoliosis (ICD-9-CM of 373). The majority of these, or 140,200 patients, were diagnosed as idiopathic scoliosis or scoliosis of unknown cause. Hospitalization with a scoliosis diagnosis was higher among the elderly, with those 65 and older accounting for nearly half (43%) among all ages. Females accounted for nearly three-quarters (73%) of all scoliosis hospitalizations. Race/ethnicity and region in the US did not show significant differences. (Reference Table 2B.2.1 PDF [177] CSV [178], Table 2B.2.2 PDF [190] CSV [191], Table 2B.2.3 PDF [208] CSV, [209] Table 2B.2.4 PDF [210] CSV [211])
In 2013, more than one-half (53.6%) of patients with a diagnosis of acquired/secondary scoliosis had a surgical procedure, but only one in five (20.7%) of those with a diagnosis of idiopathic scoliosis had surgery. The most common procedure performed on scoliosis patients was spinal fusion, with 26,600, or 16%, having this procedure. A majority of scoliosis patients with a fusion procedure (83%) had fusion of 4 or more levels. Sex of the patient was not a factor in having a procedure, but persons age 45 to 64 were most likely to have a procedure. (Reference Table 2B.5.0.1 PDF [212] CSV [213], Table 2B.5.0.2 PDF [214] CSV [215], Table 2B.5.1 PDF [216] CSV [217], Table 2B.5.2 PDF [194] CSV [195])
The cost of care for adults with scoliosis includes direct costs and indirect costs of lost wages, time away from work, cost of care providers, and opportunity costs. Estimates of the direct costs of nonsurgical care in adult scoliosis are estimated to be as high as $14,000 per year.10 The national mean cost of a hospitalization, including surgical treatment, for patients with a primary diagnosis of idiopathic scoliosis was $69,400 in 2013 for an average hospital stay of 5.3 days. The mean cost for those with an acquired or secondary scoliosis diagnosis were significantly higher at $120,400 per discharge, with an average stay of 5.9 days. The HCUP NIS database does not provide hospitalization costs associated with secondary discharge diagnoses, and does not include fees to doctors, tests, and other typical charges associated with hospitalization. Therefore, the most conservative estimate of only the hospitalization cost for adult scoliosis, both idiopathic and acquired/secondary in 2013 was an estimated $11.5 billion (166,600 hospitalizations). Charges are not necessarily actual costs paid. Mean charges for scoliosis diagnosed patients are significantly higher than for all hospital discharge patients. (Reference Table 2B.3.2 PDF [198] CSV [199])
In 2013, slightly more than one-half (58%) of patients with a scoliosis diagnosis were discharged to home, while 70% of patients with any diagnosis had a routine discharge. Patients with a scoliosis diagnosis are more likely to be transferred to a skilled nursing or intermediate care facility (long-term care) than are patients with all diagnoses. This is particularly true for the elderly population, with 39% of persons age 65 and older with a scoliosis diagnosis moving to a long-term care facility. (Reference Table 2B.4.2 PDF [204] CSV [205])
The real cost of the management of adult scoliosis to our healthcare system is significant, and the value of care measured by change in health status remains incompletely defined for both nonsurgical and surgical care.
Recent emphasis has been placed on sagittal plane balance and restoring normal sagittal alignment with regards to the three dimensional deformity of adult spinal deformity (ASD), and is a primary condition leading to the high prevalence (68%) of persons age 60 and over with adult spinal deformity.1,2 The impact of sagittal plane alignment on the treatment of spinal disorders is of critical importance. A failure to recognize malalignment in this plane can have significant consequences for the patient not only for pain and deformity, but also social interaction due to deficient forward gaze. A good understanding of the principles of sagittal balance is vital to achieve optimum outcomes when treating spinal disorders. Even when addressing problems in the coronal plane (front from back), an awareness of sagittal balance is necessary to avoid future complications.3
Sagittal plane deformity presents as an exaggeration or deficiency of normal lumbar lordosis (inward curving of the lumbar spine just above the buttocks) or kyphosis (exaggerated curvature of the upper (thoracic) spine). There are variations on the degree of normal curvature, still this shape allows equal distribution of forces across the spinal column. It is the disruption of this equilibrium by pathological processes or, as in most cases, ageing that results in deformity. This leads to adaptive changes in the pelvis and lower limbs. The effects of limb alignment on spinal posture are well documented. Changes in pelvic posture also affect spinal alignment.3
A lordosis deformity is usually iatrogenic (illness or condition caused by medication or treatment), and often follows lumbar fusion, thoracolumbar fusion, and, in some cases, lumbar decompressive procedures. Nonsurgical causes include ankylosing spondylitis, degenerative changes, or adult presentation of adolescent idiopathic scoliosis. The deformity may lead to neurogenic radicular symptoms secondary to stenosis, paraspinal muscular fatigue, and low back pain. Nonoperative treatment options fail for most patients. Surgical interventions are aimed at restoring lumbar lordosis, which is typically accomplished with revision decompression, fusion, and various osteotomies.4
Kyphosis is often secondary to inflammatory, degenerative, or post- traumatic disorders, and can be caused by poor posture, slouching, osteoporosis, birth defects, or disease. They may also be secondary to infection or tumors. There is usually pain and functional disability along with concerns about self-image and social interaction due to inability to maintain a horizontal gaze. The resultant pelvic and lower limb posture is an attempt to restore normal alignment. Addressing this complex problem requires detailed expertise and awareness of the potential pitfalls surrounding its treatment.1
Increasingly positive sagittal imbalance has been shown to correlate with poor functional outcome and poor self-image along with poor psychological function. Restoring normal spinopelvic alignment is paramount to the treatment of complex spinal deformity with sagittal imbalance. Understanding of whole spinal alignment and dynamics of spinopelvic alignment is essential to restore sagittal balance while minimizing the risk of developing sagittal decompensation after surgical intervention.1,3
The goal of sagittal deformity management is to maintain the body in an energy-efficient, ergonomically favorable erect position. The larger the deviation from a balanced alignment, the more energy an individual uses to stand upright without external suport. Patients with symptomatic sagittal plane deformity often present with a sagittal balance at the periphery of this balanced alignment, leading to an increased effort of accessory musculature to maintain the head over the pelvis. This leads to fatigue and pain, especially with prolonged activity. As sagittal imbalance progresses, different compensatory mechanisms such as the pelvic retroversion, hip extension, and knee flexion are used in order to restore and maintain sagittal balance. Once a spinal deformity surpasses these compensatory mechanisms surgical intervention is often requested.5
Operative management of sagittal deformity in the adult encompasses a spectrum of procedures with fusion the most common. In 2013, a query of the Healthcare Costs and Utilization Project (HCUP) Nationwide Inpatient Survey (NIS) resulted in approximately 190,500 hospitalizations associated with a discharge diagnosis of sagittal deformity. The largest share (76%), or 144,600 patients, were diagnosed with spondylolisthesis. Hospitalization with a sagittal deformity diagnosis was higher among the elderly, accounting for more than one-half (54%) among all ages for those 65 and older. Females accounted for 69% of all sagittal deformity hospitalizations. Race/ethnicity and region in the US did not show significant differences. (Reference Table 2B.2.1 PDF [177] CSV [178], Table 2B.2.2 PDF [190] CSV [191], Table 2B.2.3 PDF [208] CSV [209], Table 2B.2.4 PDF [210] CSV [211])
In 2013, more than nearly three-fourths (72.3%) of patients with a diagnosis of sagittal deformity had a surgical procedure. A diagnosis of spondylolisthesis had the highest rate (84.6%) of surgical procedure. The most common procedure performed on sagittal deformity patients was spinal fusion, with 67.4%, having this procedure. More than one-half (56%) had fusion of less than four levels. Sex of the patient was not a factor in having a procedure, but persons age 45 to 64 were most likely to have a procedure. (Reference Table 2B.5.0.1 PDF [212] CSV [213], Table 2B.5.0.2 PDF [214] CSV [215], Table 2B.5.1 PDF [216] CSV [217], Table 2B.5.2 PDF [194] CSV [195])
Sagittal balance is an independent predictor of clinical outcomes in spinal care. Surgical treatment is challenging and jeopardized by frequent complications. Guidelines for surgical treatment are currently not based on a classification of the disease. A comprehensive classification of sagittal balance based on regional deformities and compensatory mechanisms combined in deformity patterns is proposed. Though the sagittal shape of the spine can change due to degeneration or trauma, correlations between sagittal shape parameters and pelvic incidence (PI) have been described. PI is not changed by degeneration, thus representing a permanent source of information on the original sagittal shape of the spine.6
The national mean cost of a hospitalization, including surgical treatment, for patients with a primary diagnosis of sagittal imbalance was $94,500 in 2013 for an average hospital stay of 4.3 days. The HCUP NIS database does not provide hospitalization costs associated with secondary discharge diagnoses, and does not include fees to doctors, tests, and other typical charges associated with hospitalization. Therefore, the most conservative estimate of only hospital charges for adult sagittal imbalance in 2013 was an estimated $18.0 billion (166,600 hospitalizations). Charges are not necessarily actual costs paid. Mean charges for sagittal imbalance diagnosed patients are significantly higher than for all hospital discharge patients. (Reference Table 2B.3.2 PDF [198] CSV [199])
In 2013, slightly more one-half (56%) of patients with a sagittal imbalance diagnosis were discharged to home, compared to 70% of patients with any diagnosis. Patients with a sagittal imbalance diagnosis are more likely to be transferred to a skilled nursing or intermediate care facility (long-term care) than are patients with all other diagnoses. This is particularly true for the elderly population, with 36% of persons age 65 and older with a sagittal imbalance diagnosis moving to a long-term care facility. (Reference Table 2B.4.2 PDF [204] CSV [205])
The real cost of the management of adult sagittal imbalance to our healthcare system is significant, and the value of care measured by change in health status remains incompletely defined for both nonsurgical and surgical care.
Spinal deformity can be caused by congenital conditions and due to aging wear and tear on the back. Medical conditions and poor bone quality may also contribute to spinal deformity, however, in many cases the cause remains unknown.
Several conditions known to contribute to spinal deformity were examined as cross diagnoses with spinal deformity at the time of a healthcare visit. The most frequent diagnosis with one in ten (9.3%) hospital discharges and a scoliosis diagnosis was congenital spinal disorders. Four other conditions – trauma/spinal fractures, spinal infections, spondylopathies, and complications of surgery – were found in less than 2% of scoliosis and between 2% and 4% of sagittal imbalance hospital discharge diagnoses. Looking at all healthcare resources, the cross-diagnosis of spinal deformity and a contributing cause dropped to 0.3% among scoliosis discharges and 0.2% among sagittal imbalance visits. (Reference Table 2B.6.0 PDF [234] CSV [235])
Several studies have examined the relationship between spinal deformity and contributing causes, but until identification of multiple conditions is made, no clear relationship can be established.
The burden of spinal deformity includes healthcare costs, pain management, therapy, alternative care, and lost workdays due to pain. The total cost of spinal deformity is difficult to determine because hospital charges are the only expenditures available in the databases. In addition, not all persons suffering from spinal deformity seek medical care.
In 2013, charges for 357,000 hospital discharges for spinal deformity were $29.5 billion. Spinal deformity charges accounted for 2.1% of all hospital charges in 2013, but only 1% of hospital discharges. (Reference Table 2B.3.1 PDF [238] CSV [239])
In addition to direct and indirect costs, persons afflicted with spinal deformity experience a reduced quality of life, which may include major constraints on mobility and activity for those with the most serious conditions.
While technical outcomes of surgery are well known and show obvious benefits for those with significant deformity, long-term health related outcomes have yet to be precisely documented. The lack of quality, long-term studies of sufficient size hampers our understanding of the mortality and morbidity rates for patients with congenital and idiopathic scoliosis, with and without treatment. Fifty years of follow-up studies of children and adolescents with untreated scoliosis have shown conflicting results, with some studies indicating a higher risk of mortality and respiratory compromise.1,2
Another study shows compromise only in patients with early reduced lung function and a large curvature.3 Yet another study has shown no differences in untreated childhood scoliosis and a control group.4 Several articles from the 1960s and one recent article report that low back pain does not occur more frequently in untreated scoliosis patients than in the general population4,5,6 unless the curvature is greater than 40°.7,8 It has also been shown that persons treated with surgery rather than bracing for adolescent idiopathic scoliosis have less pain at 10- to 20-year follow-up, although function remains similar.9,10 The cosmetic/self-image aspect of scoliosis is obvious and important, and often a major factor affecting the lives of individuals with this condition.
Scoliosis in the adult has an impact that is similar to other common medical conditions including osteoarthritis, coronary artery disease, and chronic obstructive pulmonary disease. Overall, the burden of scoliosis on health-related quality of life is severe relative to other common medical conditions. With the aging demographic profile of the US, the burden of adult scoliosis is increasing and has a significant impact on the health of our population, and on the cost of care for spinal disorders.
Likewise, vertebral compression fractures, which may contribute to adult degenerative scoliosis, are also a growing concern for the aging population, particularly when associated with kyphosis and/or disabling pain.
With the sagittal profile of the spine, conventional thinking has been to categorize it into different segments based on the anatomical differentiation of the vertebrae. This delineation does not take into account the true surface contour of the spine. The disadvantage of this overly simplistic categorization is that when attempting to restore what is perceived as a ‘normal thoracolumbar spine,’ a ‘one size fits all’ approach is used.1
Increased understanding of sagittal plane deformity will lead to earlier identification. As the life expectancy of the population increases along with the patients desire to lead more active lives well into advanced years, so will the demand for appropriate expertise and skill in dealing with this complex problem. Spinal osteotomies remain complicated procedures. This treatment strategy must be the subject of specific training and must be practiced by specialist surgeons for the best outcomes.1
Curvature of Spine:
Idiopathic Scoliosis: 737.30-737.32
Acquired Kyphosis and Lordosis: 737.0, 737.10, 737.12, 737.19, 737.20-737.29, 737.34, 737.39
Secondary Scoliosis, Kyphosis, and Lordosis: 737.11, 737.33, 737.40-737.43, 737.8, 737.9
Spondylolisthesis: 737.40, 756.12
Adolescent Postural Kyphosis: 737.00
Kyphosis: 737.10-737.19, 737.41
Lordosis: 737.20-737.29, 737.42
Scoliosis: 737.30-737.39, 737.40, 737.43, 737.8, 737.9
Trauma: Spinal Fractures Contributing to Deformity:
Vertebral Compression Fractures: 805.00-805.08, 805.2, 805.4, 805.6, 805.8
Traumatic Fractures: 805.10-805.18, 805.3, 805.5, 805.7, 805.9, 806.00-806.09, 806.10-806.19, 806.20-806.29,806.30-806.39, 806.4, 806.5, 806.60-806.02, 806.69, 806.70-806.72, 806.79, 806.8, 806.9
Infection/Complications Codes:
Tuberculosis of Vertical Column: 015.00 to 015.06
Tuberculosis Unspecified: 015.90 to 015.96
Intracranial and Intraspinal Abscess (Epidural abscess): 324.1, 324.9
Acute Osteomyelitis: 730.00, 730.08, 730.09
Chronic Osteomyelitis: 730.10, 730.18, 730.19
Discitis: 722.90 to 722.93
Complications of Surgery: 996.2, 996.59, 996.63, 996.72
Spondylopathies:
Ankylosing Spondylitis: 720.00
Spinal Enthesopathy: 720.1
Sacroiliitis, not elsewhere classified: 720.2
Other Inflammatory Spondylopathies: 720.81, 820.89
Unspecified Inflammatory Spondylopathy: 720.9
Cervical Spondylosis with Myelopathy: 721.1
Thoracic or Lumbar Spondylosis with Myelopathy: 721.4
Spondylosis with Myelopathy, Thoracic Region: 721.41
Spondylosis with Myelopathy, Lumbar Region: 721.42
Intervertebral Disc Disorder with Myelopathy: 722.70 to 722.73
Spinal Stenosis in Cervical Region: 723.00
Cervicalgia: 723.1
Cervicocranial Syndrome: 723.2
Cervicobrachial Syndrome (diffuse): 723.3
Brachial Neuritis or Radiculitis NOS: 723.4
Torticollis, Unspecified: 723.5
Panniculitis Specified as Affecting Neck: 723.6
Ossification of Posterior Longitudinal Ligament in Cervical Region: 723.7
Spinal Deformity Procedures:
Decompression: 0309, 8050, 8051
Cervical Fusion: 8102, 8103
Thoracic/Dorsal or Dorsolumbar Fusion: 8104, 8105
Lumbar and Lumbosacral Fusion: 8106, 8107, 8108
Other Fusion: 8100, 8101
Cervical Refusion: 8132, 8133
Thoracic, Dorsal or Dorsolumbar Refusion: 8134, 8135
Lumbar and Lumbosacral Refusion: 8136, 8137, 8138
Other Refusion: 8130, 8131, 8139
Fusion/Refusion of Multiple Vertebrae: 8162, 8163, 8164
Instrumentation/Insertion of Spinal Device: 8451, 8452, 8459
Vertebraplasty: 8165
Kyphoplasty [Percutaneous Vertebral Augmentation]: 8166 Decompression: 0309
Diskectomy: 8050, 8051
Epidural injection: 8192, 8396, 8397
Links:
[1] http://www.boneandjointburden.org/fourth-edition/iia0/low-back-and-neck-pain
[2] http://www.boneandjointburden.org/fourth-edition/iib0/spinal-deformity
[3] https://bmus.latticegroup.com/docs/bmus_e4_t2a.5.pdf
[4] https://bmus.latticegroup.com/docs/bmus_e4_t2a.5.csv
[5] https://bmus.latticegroup.com/docs/bmus_e4_t2a.1.pdf
[6] https://bmus.latticegroup.com/docs/bmus_e4_t2a.1.csv
[7] https://bmus.latticegroup.com/file/bmuse4g201png
[8] https://bmus.latticegroup.com/docs/bmus_e4_g2.0.1.png
[9] https://bmus.latticegroup.com/file/bmuse4g202png
[10] https://bmus.latticegroup.com/docs/bmus_e4_g2.0.2.png
[11] https://bmus.latticegroup.com/docs/bmus_e4_t2a.11.1.pdf
[12] https://bmus.latticegroup.com/docs/bmus_e4_t2a.11.1.csv
[13] https://bmus.latticegroup.com/docs/bmus_e4_T8.6.2.pdf
[14] https://bmus.latticegroup.com/docs/bmus_e4_T8.6.2.csv
[15] https://bmus.latticegroup.com/docs/bmus_e4_t2a.2.1.pdf
[16] https://bmus.latticegroup.com/docs/bmus_e4_t2a.2.1.csv
[17] https://bmus.latticegroup.com/file/bmuse4g2a01png
[18] https://bmus.latticegroup.com/docs/bmus_e4_g2a.0.1.png
[19] https://bmus.latticegroup.com/docs/bmus_e4_t2a.4.1.pdf
[20] https://bmus.latticegroup.com/docs/bmus_e4_t2a.4.1.csv
[21] https://bmus.latticegroup.com/file/bmuse4g2b01png
[22] https://bmus.latticegroup.com/docs/bmus_e4_g2b.0.1.png
[23] https://bmus.latticegroup.com/docs/bmus_e4_t2a.2.2.pdf
[24] https://bmus.latticegroup.com/docs/bmus_e4_t2a.2.2.csv
[25] https://bmus.latticegroup.com/file/bmuse4g2b02png
[26] https://bmus.latticegroup.com/docs/bmus_e4_g2b.0.2.png
[27] https://bmus.latticegroup.com/file/bmuse4g2b03png
[28] https://bmus.latticegroup.com/docs/bmus_e4_g2b.0.3.png
[29] https://bmus.latticegroup.com/file/bmuse4g2b04png
[30] https://bmus.latticegroup.com/docs/bmus_e4_g2b.0.4.png
[31] https://bmus.latticegroup.com/docs/bmus_e4_t2a.2.3.pdf
[32] https://bmus.latticegroup.com/docs/bmus_e4_t2a.2.3.csv
[33] https://bmus.latticegroup.com/docs/bmus_e4_t2a.2.4.pdf
[34] https://bmus.latticegroup.com/docs/bmus_e4_t2a.2.4.csv
[35] https://bmus.latticegroup.com/docs/bmus_e4_t2a.8.pdf
[36] https://bmus.latticegroup.com/docs/bmus_e4_t2a.8.csv
[37] https://bmus.latticegroup.com/docs/bmus_e4_t2a.9.pdf
[38] https://bmus.latticegroup.com/docs/bmus_e4_t2a.9.csv
[39] https://bmus.latticegroup.com/docs/bmus_e4_t2a.10.1.pdf
[40] https://bmus.latticegroup.com/docs/bmus_e4_t2a.10.1.csv
[41] https://bmus.latticegroup.com/docs/bmus_e4_t2a.10.2.pdf
[42] https://bmus.latticegroup.com/docs/bmus_e4_t2a.10.2.csv
[43] https://bmus.latticegroup.com/docs/bmus_e4_t2a.10.3.pdf
[44] https://bmus.latticegroup.com/docs/bmus_e4_t2a.10.3.csv
[45] https://bmus.latticegroup.com/docs/bmus_e4_t2a.10.4.pdf
[46] https://bmus.latticegroup.com/docs/bmus_e4_t2a.10.4.csv
[47] https://bmus.latticegroup.com/file/bmuse4g2b05png
[48] https://bmus.latticegroup.com/docs/bmus_e4_g2b.0.5.png
[49] https://bmus.latticegroup.com/file/bmuse4g2b06png
[50] https://bmus.latticegroup.com/docs/bmus_e4_g2b.0.6.png
[51] https://bmus.latticegroup.com/file/bmuse4g2c011png
[52] https://bmus.latticegroup.com/docs/bmus_e4_g2c.0.1.1.png
[53] https://bmus.latticegroup.com/docs/bmus_e4_t2a.3.1.pdf
[54] https://bmus.latticegroup.com/docs/bmus_e4_t2a.3.1.csv
[55] https://bmus.latticegroup.com/file/bmuse4g2c012png
[56] https://bmus.latticegroup.com/docs/bmus_e4_g2c.0.1.2.png
[57] https://bmus.latticegroup.com/docs/bmus_e4_t2a.3.2.pdf
[58] https://bmus.latticegroup.com/docs/bmus_e4_t2a.3.2.csv
[59] https://bmus.latticegroup.com/file/bmuse4g2c02png
[60] https://bmus.latticegroup.com/docs/bmus_e4_g2c.0.2.png
[61] https://bmus.latticegroup.com/file/bmuse4g2c03png
[62] https://bmus.latticegroup.com/docs/bmus_e4_g2c.0.3.png
[63] https://bmus.latticegroup.com/file/bmuse4g2c04png
[64] https://bmus.latticegroup.com/docs/bmus_e4_g2c.0.4.png
[65] https://bmus.latticegroup.com/docs/bmus_e4_t2a.3.3.pdf
[66] https://bmus.latticegroup.com/docs/bmus_e4_t2a.3.3.csv
[67] https://bmus.latticegroup.com/docs/bmus_e4_t2a.3.4.pdf
[68] https://bmus.latticegroup.com/docs/bmus_e4_t2a.3.4.csv
[69] https://bmus.latticegroup.com/file/bmuse4g2c05png
[70] https://bmus.latticegroup.com/docs/bmus_e4_g2c.0.5.png
[71] https://bmus.latticegroup.com/file/bmuse4g2c06png
[72] https://bmus.latticegroup.com/docs/bmus_e4_g2c.0.6.png
[73] https://bmus.latticegroup.com/file/bmuse4g2d01png
[74] https://bmus.latticegroup.com/docs/bmus_e4_g2d.0.1.png
[75] https://bmus.latticegroup.com/docs/bmus_e4_t2a.4.2.pdf
[76] https://bmus.latticegroup.com/docs/bmus_e4_t2a.4.2.csv
[77] https://bmus.latticegroup.com/docs/bmus_e4_t2a.4.3.pdf
[78] https://bmus.latticegroup.com/docs/bmus_e4_t2a.4.3.csv
[79] https://bmus.latticegroup.com/docs/bmus_e4_t2a.4.4.pdf
[80] https://bmus.latticegroup.com/docs/bmus_e4_t2a.4.4.csv
[81] https://bmus.latticegroup.com/docs/bmus_e4_t2a.6.pdf
[82] https://bmus.latticegroup.com/docs/bmus_e4_t2a.6.csv
[83] https://bmus.latticegroup.com/docs/bmus_e4_t2a.7.1.pdf
[84] https://bmus.latticegroup.com/docs/bmus_e4_t2a.7.1.csv
[85] https://bmus.latticegroup.com/docs/bmus_e4_t2a.7.2.pdf
[86] https://bmus.latticegroup.com/docs/bmus_e4_t2a.7.2.csv
[87] https://bmus.latticegroup.com/docs/bmus_e4_t2a.7.3.pdf
[88] https://bmus.latticegroup.com/docs/bmus_e4_t2a.7.3.csv
[89] https://bmus.latticegroup.com/docs/bmus_e4_t2a.7.4.pdf
[90] https://bmus.latticegroup.com/docs/bmus_e4_t2a.7.4.csv
[91] https://bmus.latticegroup.com/file/bmuse4g2d02png
[92] https://bmus.latticegroup.com/docs/bmus_e4_g2d.0.2.png
[93] https://bmus.latticegroup.com/file/bmuse4g2d03png
[94] https://bmus.latticegroup.com/docs/bmus_e4_g2d.0.3.png
[95] https://bmus.latticegroup.com/docs/bmus_e4_t2a.11.2.pdf
[96] https://bmus.latticegroup.com/docs/bmus_e4_t2a.11.2.csv
[97] https://bmus.latticegroup.com/docs/bmus_e4_t2a.11.3.pdf
[98] https://bmus.latticegroup.com/docs/bmus_e4_t2a.11.3.csv
[99] https://bmus.latticegroup.com/docs/bmus_e4_t2a.11.4.pdf
[100] https://bmus.latticegroup.com/docs/bmus_e4_t2a.11.4.csv
[101] https://bmus.latticegroup.com/docs/bmus_e4_t2a.12.pdf
[102] https://bmus.latticegroup.com/docs/bmus_e4_t2a.12.csv
[103] https://bmus.latticegroup.com/docs/bmus_e4_t2a.13.1.pdf
[104] https://bmus.latticegroup.com/docs/bmus_e4_t2a.13.1.csv
[105] https://bmus.latticegroup.com/file/bmuse4g2d041png
[106] https://bmus.latticegroup.com/docs/bmus_e4_g2d.0.4.1.png
[107] https://bmus.latticegroup.com/docs/bmus_e4_t2a.13.2.pdf
[108] https://bmus.latticegroup.com/docs/bmus_e4_t2a.13.2.csv
[109] https://bmus.latticegroup.com/docs/bmus_e4_t2a.13.3.pdf
[110] https://bmus.latticegroup.com/docs/bmus_e4_t2a.13.3.csv
[111] https://bmus.latticegroup.com/docs/bmus_e4_t2a.13.4.pdf
[112] https://bmus.latticegroup.com/docs/bmus_e4_t2a.13.4.csv
[113] https://bmus.latticegroup.com/file/bmuse4g2d051png
[114] https://bmus.latticegroup.com/docs/bmus_e4_g2d.0.5.1.png
[115] https://bmus.latticegroup.com/file/bmuse4g2d042png
[116] https://bmus.latticegroup.com/docs/bmus_e4_g2d.0.4.2.png
[117] https://bmus.latticegroup.com/file/bmuse4g2d052png
[118] https://bmus.latticegroup.com/docs/bmus_e4_g2d.0.5.2.png
[119] https://bmus.latticegroup.com/docs/bmus_e4_t2a.15.pdf
[120] https://bmus.latticegroup.com/docs/bmus_e4_t2a.15.csv
[121] https://bmus.latticegroup.com/file/bmuse4g2e01png
[122] https://bmus.latticegroup.com/docs/bmus_e4_g2e.0.1.png
[123] https://bmus.latticegroup.com/docs/bmus_e4_t2a.14.pdf
[124] https://bmus.latticegroup.com/docs/bmus_e4_t2a.14.csv
[125] https://bmus.latticegroup.com/file/bmuse4g2e02png
[126] https://bmus.latticegroup.com/docs/bmus_e4_g2e.0.2.png
[127] https://bmus.latticegroup.com/docs/bmus_e4_t2a.16.1.pdf
[128] https://bmus.latticegroup.com/docs/bmus_e4_t2a.16.1.csv
[129] https://bmus.latticegroup.com/file/bmuse4g2e03png
[130] https://bmus.latticegroup.com/docs/bmus_e4_g2e.0.3.png
[131] https://bmus.latticegroup.com/docs/bmus_e4_t2a.16.2.pdf
[132] https://bmus.latticegroup.com/docs/bmus_e4_t2a.16.2.csv
[133] https://bmus.latticegroup.com/file/bmuse4g2e04png
[134] https://bmus.latticegroup.com/docs/bmus_e4_g2e.0.4.png
[135] https://bmus.latticegroup.com/file/bmuse4g2e05png
[136] https://bmus.latticegroup.com/docs/bmus_e4_g2e.0.5.png
[137] https://bmus.latticegroup.com/docs/bmus_e4_t2a.17.pdf
[138] https://bmus.latticegroup.com/docs/bmus_e4_t2a.17.csv
[139] https://bmus.latticegroup.com/file/bmuse4g2e06png
[140] https://bmus.latticegroup.com/docs/bmus_e4_g2e.0.6.png
[141] https://bmus.latticegroup.com/docs/bmus_e4_t2a.18.pdf
[142] https://bmus.latticegroup.com/docs/bmus_e4_t2a.18.csv
[143] https://bmus.latticegroup.com/file/bmuse4g2e07png
[144] https://bmus.latticegroup.com/docs/bmus_e4_g2e.0.7.png
[145] https://bmus.latticegroup.com/docs/bmus_e4_t2a.19.pdf
[146] https://bmus.latticegroup.com/docs/bmus_e4_t2a.19.csv
[147] https://bmus.latticegroup.com/docs/bmus_e4_t2a.20.pdf
[148] https://bmus.latticegroup.com/docs/bmus_e4_t2a.20.csv
[149] https://bmus.latticegroup.com/file/bmuse4g2e08png
[150] https://bmus.latticegroup.com/docs/bmus_e4_g2e.0.8.png
[151] https://bmus.latticegroup.com/docs/bmus_e4_t2a.21.pdf
[152] https://bmus.latticegroup.com/docs/bmus_e4_t2a.21.csv
[153] https://bmus.latticegroup.com/file/bmuse4g2f01png
[154] https://bmus.latticegroup.com/docs/bmus_e4_g2f.0.1.png
[155] https://bmus.latticegroup.com/docs/bmus_e4_T8.12.pdf
[156] https://bmus.latticegroup.com/docs/bmus_e4_T8.12.csv
[157] https://bmus.latticegroup.com/file/bmuse4g2g01png
[158] https://bmus.latticegroup.com/docs/bmus_e4_g2g.0.1.png
[159] https://bmus.latticegroup.com/docs/bmus_e4_T8.2.2.pdf
[160] https://bmus.latticegroup.com/docs/bmus_e4_T8.2.2.csv
[161] https://bmus.latticegroup.com/file/bmuse4g2g02png
[162] https://bmus.latticegroup.com/docs/bmus_e4_g2g.0.2.png
[163] https://bmus.latticegroup.com/docs/bmus_e4_T8.4.2.pdf
[164] https://bmus.latticegroup.com/docs/bmus_e4_T8.4.2.csv
[165] https://bmus.latticegroup.com/file/bmuse4g2g03png
[166] https://bmus.latticegroup.com/docs/bmus_e4_g2g.0.3.png
[167] https://bmus.latticegroup.com/file/bmuse4g2g04png
[168] https://bmus.latticegroup.com/docs/bmus_e4_g2g.0.4.png
[169] https://bmus.latticegroup.com/file/bmuse4g2g05png
[170] https://bmus.latticegroup.com/docs/bmus_e4_g2g.0.5.png
[171] http://www.boneandjointburden.org/fourth-edition/iiaf0/economic-burden
[172] https://bmus.latticegroup.com/docs/bmus_e4_spine%20ICD-9%20to%20ICD-10.pdf
[173] https://bmus.latticegroup.com/docs/bmus_e4_T2B.1.0.pdf
[174] https://bmus.latticegroup.com/docs/bmus_e4_T2B.1.0.csv
[175] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.0.pdf
[176] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.0.csv
[177] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.1.pdf
[178] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.1.csv
[179] https://bmus.latticegroup.com/file/bmuse4g2b210png
[180] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.0.png
[181] https://bmus.latticegroup.com/file/cobb-anglepng
[182] https://bmus.latticegroup.com/docs/cobb-angle.png
[183] https://bmus.latticegroup.com/file/adolescent-prevalencepng
[184] https://bmus.latticegroup.com/docs/adolescent%20prevalence.png
[185] https://bmus.latticegroup.com/file/congenital-scoliosis-syndromespng
[186] https://bmus.latticegroup.com/docs/congenital%20scoliosis%20syndromes.png
[187] https://www.srs.org/patients-and-families/conditions-and-treatments/parents/scoliosis
[188] http://www.ncbi.nlm.nih.gov/pubmed/15931035
[189] http://www.wheelessonline.com/ortho/congenital_scoliosis_and_vertebral_defects
[190] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.2.pdf
[191] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.2.csv
[192] https://bmus.latticegroup.com/file/bmuse4g2b211png
[193] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.1.png
[194] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.2.pdf
[195] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.2.csv
[196] https://bmus.latticegroup.com/file/bmuse4g2b212png
[197] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.2.png
[198] https://bmus.latticegroup.com/docs/bmus_e4_T2B.3.2.pdf
[199] https://bmus.latticegroup.com/docs/bmus_e4_T2B.3.2.csv
[200] https://bmus.latticegroup.com/file/bmuse4g2b213png
[201] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.3.png
[202] https://bmus.latticegroup.com/file/bmuse4g2b214png
[203] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.4.png
[204] https://bmus.latticegroup.com/docs/bmus_e4_T2B.4.2.pdf
[205] https://bmus.latticegroup.com/docs/bmus_e4_T2B.4.2.csv
[206] https://bmus.latticegroup.com/file/bmuse4g2b221png
[207] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.2.1.png
[208] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.3.pdf
[209] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.3.csv
[210] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.4.pdf
[211] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.4.csv
[212] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.0.1.pdf
[213] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.0.1.csv
[214] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.0.2.pdf
[215] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.0.2.csv
[216] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.1.pdf
[217] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.1.csv
[218] https://bmus.latticegroup.com/file/bmuse4g2b222png
[219] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.2.2.png
[220] https://bmus.latticegroup.com/file/bmuse4g2b223png
[221] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.2.3.png
[222] https://bmus.latticegroup.com/file/bmuse4g2b224png
[223] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.2.4.png
[224] https://bmus.latticegroup.com/file/sagittal-plane-deformitypng
[225] https://bmus.latticegroup.com/docs/sagittal%20plane%20deformity.png
[226] https://bmus.latticegroup.com/file/bmuse4g2b31png
[227] https://bmus.latticegroup.com/docs/bmus_e4_g2b.3.1.png
[228] https://bmus.latticegroup.com/file/bmuse4g2b32png
[229] https://bmus.latticegroup.com/docs/bmus_e4_g2b.3.2.png
[230] https://bmus.latticegroup.com/file/bmuse4g2b33png
[231] https://bmus.latticegroup.com/docs/bmus_e4_g2b.3.3.png
[232] https://bmus.latticegroup.com/file/bmuse4g2b34png
[233] https://bmus.latticegroup.com/docs/bmus_e4_g2b.3.4.png
[234] https://bmus.latticegroup.com/docs/bmus_e4_T2B.6.0.pdf
[235] https://bmus.latticegroup.com/docs/bmus_e4_T2B.6.0.csv
[236] https://bmus.latticegroup.com/file/bmuse4g2b41png
[237] https://bmus.latticegroup.com/docs/bmus_e4_g2b.4.1.png
[238] https://bmus.latticegroup.com/docs/bmus_e4_T2B.3.1.pdf
[239] https://bmus.latticegroup.com/docs/bmus_e4_T2B.3.1.csv