 [8]
[8] 

A normal spine is structurally balanced for optimal flexibility and has gentle front-to-back inward and outward curves that work in harmony to keep the body’s center of gravity aligned over the hips and pelvis. The cervical spine (neck) and lumbar (lower) spine both have a lordosis, an inward or concave curve, while the thoracic (middle) spine has a kyphosis, an outward or convex curve. Together these curves form a gentle S.
Spinal deformity is caused by abnormal curvature of the spine putting it out of alignment. When the abnormal curvature is seen from the side (a front-to-back imbalance) it is called sagittal imbalance, and includes the conditions of kyphosis, lordosis, and spondylolisthesis resulting in flatback syndrome and chin-on-chest or dropped head syndrome. When seen from the back (a side-to-side imbalance) it is called scoliosis. While scoliosis can be caused by conditions such as cerebral palsy, muscular dystrophy, and a broad spectrum of conditions (acquired or secondary scoliosis), the cause of most scoliosis is unknown (idiopathic scoliosis). Spinal deformity affects individuals in every age and demographic group, but the prevalence increases with age as many causes are affected by degenerative conditions.
Spinal deformity has a significant and measurable impact on health-related quality of life, including pain, function, self-image, mental health, work status, and disability. Prevalence of disease, utilization of healthcare resources, impact of disease on health-related quality of life, and cost of care are useful tools for measuring the burden of deformity on our population and on our healthcare economy. The purpose of this chapter is to provide information on the burden of spinal deformity on patients and on our healthcare system.
Adult spinal deformity is a broad diagnostic classification that includes idiopathic scoliosis as well as de novo or degenerative curves, which often result in coronal and/or sagittal plane decompensation. Sagittal plane malalignment is an increasingly recognized cause of pain and disability.1
The prevalence of spinal deformity has been reported at a wide range depending on the type of deformity and age. Congenital scoliosis has been reported at 100 in 100,000 persons,2 with acquired deformity as high as 68,000 in 100,000 persons.3 (Reference Table 2B.1.0 PDF [1] CSV [2])
Conditions related to the spine and spinal deformity often sound similar but affect the spine in different ways. Key conditions discussed in this section include the following.
Curvature of the spine: Spine curvature can refer to two distinct conditions. The human spine normally curves, but more commonly the term "spinal curvature" refers to abnormalities from the standard spinal.
• Idiopathic: Of unknown cause. Any disease that is of uncertain or unknown origin may be termed idiopathic; usually associated with children who develop an abnormal curvature at a young age.
• Acquired: Curvature that develops over many years, usually associated with adults and older persons.
• Secondary: Curvature caused by another condition, such as osteoporosis.
Sagittal imbalance: Deformity where loss of the normal lordosis of the lumbar spine or increased kyphosis of the thoracic and thoracolumbar spine causes the torso and head to pitch forward relative to the hips and pelvis. Loss of lordosis in the lumbar spine is also known as flat back syndrome.
Scoliosis: Side-to-side abnormal curvature of the spine.
Spondylolisthesis: Forward movement of one vertebra in relationship to a vertebra below it.
Spondylosis: Degeneration of the disc spaces between the vertebrae. Spondylosis is common with aging and affects virtually everyone to some degree after the age of 60 years. When severe, it can cause local pain and decreased range of spinal motion, requiring pain and/or anti-inflammatory medications.
Stenosis: A narrowing of the open spaces within the spine, which can put pressure on the spinal cord and the nerves that travel through the spine. Spinal stenosis occurs most often in the neck and lower back.
Kyphosis: An abnormal, convex curvature of the spine, with a resultant bulge at the upper, middle or lower back.
Spinal fractures:
• Traumatic spine fractures (TF): High-energy fractures resulting from accidents, falls, and sports.
• Vertebral compression fractures (VCF): Low-energy fractures in the aging as a result of reduced bone density and strength (osteoporosis and osteopenia).
Spinal infection:
• Tuberculosis of spine: An infection that usually occurs in the lungs, but can also occur in the spine, resulting in destruction of the intervertebral disk space and adjacent vertebral bodies. It is more common in children and young adults.
• Intraspinal abscess: A collection of pus and infectious material in the spine.
• Osteomylitis: A bone infection normally caused by bacteria but sometimes by fungus. The infection can occur in any bone but typically affects the arms, legs, spine, and pelvis. The bacteria usually reach the bone from an injury or wound. It can be either acute, where symptoms of pain, swelling, and fever last only a few months, or chronic.
• Discitis: Infection exists in the small spaces between these bones (the intervertebral disc spaces), which puts pressure on the discs and causes pain. Discitis is relatively uncommon and mostly affects young children.
• Postoperative infections: Infections after surgical procedures (operations) can cause pain, poor wound healing, need for further treatment including antibiotics, longer hospital stays, and increased healthcare costs.
Complications of surgery: Common surgery complications, including excessive blood loss, pain, infection, neural injury, anesthesia effects, blood clots, and other medical complications (heart attack, stroke).
Spondylopathies: Any disease of the vertebrae or of the spinal column.
Surgical procedures: Often performed to reduce pain and deformity from spinal curvature including osteotomies ( complete or partial removal of the vertebral bodies), spinal instrumentation, and fusion.
• Spinal fusion: A surgical procedure in which two or more vertebrae are permanently joined into one solid bone with no space between them.
• Osteotomies: A surgical procedure in which a portion of the vertebral body is removed to help restore the normal alignment of the spine. The procedure is utilized to reduce the amount of kyphosis or increase lordosis.
The normal spine viewed from the side forms a gentle "S" shape. When viewed from the back, the normal spine appears straight. The naturally occurring soft curves of the spine are designed to distribute mechanical stress in the body when at rest and during movement. When the curvature is even slightly abnormal, a person may experience occasional mild or annoying discomfort. If the curve is severely abnormal, the pain is usually severe and accompanied by disability. Scoliosis occurs in both children, where it is generally idiopathic, and adults, where it is often acquired.
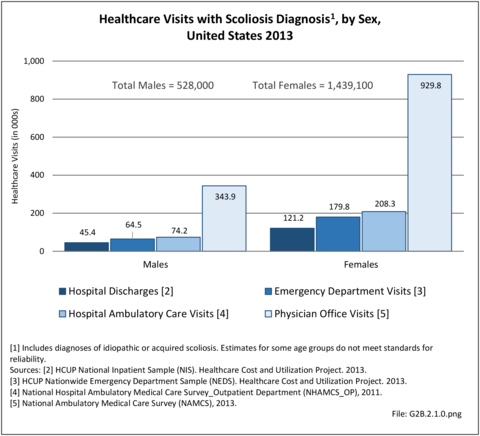
In 2013, there were nearly 2 million healthcare visits with a diagnosis of scoliosis, the majority of which 1.3 million were to a physician’s office. However, 166,600 hospital discharges had a scoliosis diagnosis. The number of hospital discharges with a scoliosis diagnosis has remained relatively steady for five years (2010 thru 2014) and represents approximately 56 persons in every 100,000 US population. Females accounted for three out of four (73%) of healthcare visits with a scoliosis diagnosis. (Reference Table 2B.2.0 PDF [3] CSV [4] and Table 2B.2.1 PDF [5] CSV [6])
Spinal deformity and scoliosis can be found at birth due to genetic causes, develop during childhood, or occur late in life because of degenerative disc and joint disease. Common signs of scoliosis are a prominent shoulder or shoulder blade, or chest wall asymmetry. Another sign is uneven hips, with one hip seemingly higher than the other hip. It is important not to confuse scoliosis with poor posture and to realize that scoliosis will usually not disappear with age. Despite the severity of these conditions and the impact they have on the lives of children, the prevalence of spinal deformities in children under the age of 18 years is difficult to determine because of relatively low numbers and the degree to which the condition manifests initially in pain or disability. Estimated prevalence of spinal deformity conditions has been cited in numerous studies, and ranges from 0.4 in 1,000 for infantile idiopathic scoliosis1 to 2.5 in 1,000 for adolescent idiopathic scoliosis.2 (Reference Table 2B.1.0 PDF [1] CSV [2])
There are several different types of scoliosis. The most common type of scoliosis is idiopathic, meaning the cause is unknown. Approximately 80% to 85% of scoliosis cases are idiopathic.3 Idiopathic scoliosis can occur as early as the first three years of life, which is known as infantile idiopathic scoliosis. If diagnosed between the ages of 4 to 10 years, it is known as juvenile idiopathic scoliosis, and from 10 years of age to skeletal maturity, as adolescent idiopathic scoliosis. The term “early onset scoliosis” (EOS) is also used to describe scoliosis that occurs prior to 10 years of age. Adolescent idiopathic scoliosis is the most common type.
Scoliosis, if severe enough (>25°), is usually treated with bracing if the child is growing or with surgery if the curvature is more severe (>45° to 50°). The standard radiograph measurement method for all forms of scoliosis is the Cobb angle measurement technique, measured from the end plates of the maximally tilted end vertebral bodies in a standing radiograph.4 Whether the curve is >25° or >40° to 45°, the treatment is preventative in nature, helping to avoid progression of the curve and more significant future problems that might occur if it was left untreated. Increased mortality has been reported in untreated early onset scoliosis due to respiratory conditions.5 While this preventative aspect is hugely valuable and intuitively important, its benefit is difficult to measure from a public health standpoint, especially for rare conditions of childhood such as juvenile and adolescent pediatric scoliosis.
Infantile scoliosis occurs in patients 0-3 years old and currently accounts for less than 1% of all cases of idiopathic scoliosis in the United States. Boys are affected by infantile idiopathic scoliosis at a higher rate than girls (3:2 ratio).1 Infantile scoliosis curves tend to be left-sided (75% to 90%). Past studies have indicated this rare type of scoliosis occurs more frequently in Europe than in North America.6
Treatment for patients with infantile idiopathic scoliosis is determined by anticipated or actual curve progression. Several common measurement techniques are used, with angles ≤20° generally considered at low risk for progression. In addition to measuring the Cobb angle, the rib-vertebra angle difference (RVAD) is used as a common predictor of curve progression.7 Patients with a Cobb angle of ≤25° and a RVAD of ≤20° are at a low risk for progression and should be re-evaluated every 4 to 6 months.1
Nonsurgical treatment, such as bracing or casting, is initiated if a curve progression of ≥10° occurs. Surgical treatment should be considered when nonsurgical measures, including both bracing and casting, are not successful. Surgical treatment is utilized when a curve is ≥45° and progressive in an immature child.1 Overall, surgical methods are continually evolving, with the goal of obtaining and maintaining curve correction while simultaneously preserving or encouraging spinal and trunk growth.
Surgical options currently utilized include various types of spinal fusion or hemiepiphysiodesis, a minimally invasive implant procedure to slow progression of curve growth. Additional techniques include growing-rod instrumentation (rods that expand and support the deformed spine) and vertical expandable (telescoping) prosthetic titanium rib (VEPTR) instrumentation.8 The goal of using surgical methods is to halt the progression of the curve and gain correction of the deformity, while allowing maximum growth of the spine, lungs, and thoracic cage.1 The allowance of normal lung development is one of the critical factors in recommending treatment for infantile and juvenile idiopathic scoliosis. Prevention of early mortality due to respiratory failure is a key driver of surgical treatment of early onset scoliosis.1,5
In 12% to 21% of idiopathic scoliosis cases, the diagnosis is made between 4 and 10 years of age. Between the ages of 4 and 6 years, the female-to-male ratio of juvenile idiopathic scoliosis is 1:1. However, the ratio of female to male cases rises to between 2:1 and 4:1 in children between the ages of 4 and 10 years, and to 8:1 in children who are 10 years of age or older.9 Both right and left curves are found with equal frequency for patients younger than 6 years, but rise to a 3:1 ratio of right versus left thoracic curves after the age of 6.10
Observation is the main treatment for patients with a small curve of less than 20° to 25°. Follow-up visits are recommended every 4, 6, 9, or 12 months, depending on the patient’s age, the degree of the curve, and the characteristics of the clinical deformity.9
Curves between 25° and 50° are usually treated with bracing in this age group. Bracing can be done either on a part- time or full-time basis, depending on the size of the curve as well as the age of the child. A study completed in 1982 evaluating the success of bracing reported an excellent prognosis when part-time bracing was utilized for patients with a curve of ≤35° and RVAD11 of ≤20°; however, curves ≥45° and RVAD of ≥20° had a less favorable prognosis for successful treatment with bracing.9
Overall, the curve patterns in patients with juvenile idiopathic scoliosis are similar to those with adolescent idiopathic scoliosis. Approximately 70% of patients with juvenile idiopathic scoliosis exhibit curve progression and require some form of treatment. In a study conducted in 1981, 55 of 98 patients (56%) with juvenile idiopathic scoliosis required spinal surgery. The most common and traditional surgery is posterior instrumentation and fusion.9
According to the Scoliosis Research Society (SRS), idiopathic scoliosis is diagnosed when a patient has asymmetry on forward bending combined with a curve of at least 10°.12 By this definition, the prevalence of adolescent idiopathic scoliosis in children from 11 to 18 years of age is 2% to 3%. Though the male-to-female ratio for smaller curves is about equal, larger curves seem to be more common in females. Similar results were found in a study conducted in 1985, where 29,195 children were screened for idiopathic scoliosis.2
Several studies have investigated the natural history and natural course of curve progression in adolescent idiopathic scoliosis. All report the strongest predictive factors in the development of idiopathic scoliosis are age, magnitude of curve, and gender.13,14,15,16 Girls are more likely to have adolescent idiopathic scoliosis than boys, and some studies report the onset is earlier in girls than boys. A factor highly correlated with curve progression is age at diagnosis; patients diagnosed at a younger age have a greater risk of curve progression. However, those diagnosed at a younger age seem to have a more favorable response to milder forms of treatment, which supports the practice of school screening to detect and lead to earlier diagnosis for those children who exhibit a smaller degree of curvature.
Treatment decisions for individuals with adolescent idiopathic scoliosis are made based on location, shape, pattern, and cause of the curve. The treatment choice is also a function of the patient’s future growth potential. Treatment choices include observation, bracing, and surgery. Observation is usually reserved for patients who have curves ≤25°. Bracing, which is used to stop curve progression (rather than for lasting correction of the curve), is usually used for patients who have curves ≥25° and who are still growing. Surgery is generally used for patients with curves ≥45°.
Congenital scoliosis is believed to affect approximately one child for every 1,000 live births.17 The cause is unknown in most cases, but in some cases, it is associated with various syndromes, as shown in the illustration below. Diagnosis occasionally is made during prenatal ultrasound. In cases of congenital scoliosis, additional congenital conditions, such as chest wall malformation or kidney or heart abnormalities, are often present. Treatment options for congenital scoliosis are bracing and/or surgery and are similar to treatments discussed for idiopathic scoliosis. Bracing is not as effective for congenital scoliosis as it is for idiopathic scoliosis.
Major abnormal spinal deformity occurring during infancy or early childhood poses a clinical problem because of the anticipated long growth period (at least 10 years), variable presentation and treatment methods, and the length of time that must pass before meaningful outcome results can be assessed in the small number of patients for definitive studies. Curves that result from congenital scoliosis are often not treated as easily as idiopathic curves because the deformity is in the bones rather than the soft tissue, causing the curve to be rigid.18
Scoliosis also occurs in conjunction with several congenital conditions that occur in infancy or childhood. These include muscular dystrophy, cerebral palsy, spina bifida, and spinal muscular atrophy. Scoliosis associated with these conditions is referred to as neuromuscular scoliosis. Both the likelihood and the severity of the scoliosis generally increases with the severity of the underlying condition. For example, a child with severe cerebral palsy who is unable to walk is more likely to have severe scoliosis than a child with mild cerebral palsy who can walk.
Because of the low prevalence of scoliosis in children and adolescents, it is difficult to analyze the healthcare impact on the US healthcare system from this condition. However, the impact of scoliosis over a lifetime due to pain, inability to work, and cost to the healthcare system are substantial.
In 2013, one in three (35%) healthcare visits with a diagnosis of scoliosis was for a person under the age of 18. Most visits, 93% of the 681,100, were classified as idiopathic scoliosis. The majority (93%) of all visits with a diagnosis of scoliosis by persons under age 18 were outpatient visits to either an outpatient clinic or physician office. Only 3.5% represented hospital discharges; however, this still accounted for 23,800 discharges for this often painful condition in children and adolescents. (Reference Table 2B.2.2 PDF [18] CSV [19])
In 2013, 40% of children and adolescents under the age of 18 years discharged from the hospital with a diagnosis of scoliosis had surgery. Spinal fusion was the most common surgery performed (36.1%), followed by incision/excision (24.6%), and deformity monitoring (9.6%). One in seven (15%) also had a blood transfusion. (Reference Table 2B.5.2 PDF [22] CSV [23])
Average hospital charges for patients under 18 years of age with a scoliosis diagnosis in 2013 were five times the average charge for all hospitalized patients in this age group ($113,800 versus $22,400), even though the length of stay was only about 50% longer (6.4 days versus 3.9 days). The high number of surgical procedures likely accounted for some of this variance. The length of stay and mean charges were slightly higher for those with an acquired/secondary scoliosis diagnoses than for those with an idiopathic scoliosis diagnosis. (Reference Table 2B.3.2 PDF [26] CSV [27])
Young people under the age of 18 with scoliosis are four times more likely to be transferred to a long-term care facility and three times more likely to have home healthcare than peers discharged for any diagnosis although the rates are still lower than among older persons (3% and 9%, respectively). (Reference Table 2B.4.2 PDF [32] CSV [33])
Deformity of the adult spine includes patients with curvature of the spine (scoliosis) of varying degrees caused or impacted by degenerative disc and joint disease. Adult scoliosis may be the result of persistent or progressive deformity since adolescence or a new, de novo, onset of deformity resulting from degeneration or aging of the spine. Degenerative scoliosis accounts for most scoliosis cases in older populations aged 65 years and older, as reflected in the low proportion of older patients with a diagnosis of primary idiopathic scoliosis.
Degenerative scoliosis is one of the most challenging spine conditions to treat because of the variability of the condition. Generally, it is thought to originate with the degeneration of the intervertebral discs, which leads to misalignment of the vertebral column. Degenerative scoliosis, particularly in the very elderly, is often associated with other conditions, such as osteoporosis. Treatment outcomes for both nonsurgical and surgical procedures are not well documented; hence, recognition and earlier intervention are important to ward off the more complex problems of adult scoliosis. The role played by undiagnosed, mild idiopathic adolescent scoliosis on the development of degenerative scoliosis in later life is unknown.
The clinical presentation and management of adults with scoliosis is characterized by a great deal of variability. There is a poor correlation between the magnitude of deformity and the impact of scoliosis on health status, as patients with large spinal curvatures may have limited pain and disability and patients with relatively mild deformity may be severely impaired. Deformity in the sagittal plane is associated with disability more than scoliosis.1 Patients with adult scoliosis seek medical care for symptoms, including back pain, neural symptoms, and progression of deformity. It is often neural symptoms secondary to spinal stenosis that leads patients to seek treatment.
The prevalence of adult spinal deformity and scoliosis is not well established, with estimates ranging from 2.5% to 25% of the population.2,3,4,5,6,7 A 2005 study reported mild to severe adult scoliosis prevalence as high as 68% in a healthy (no known scoliosis or spine surgery) population aged 60 years and older.8 Many cases of degenerative scoliosis are undiagnosed, but elderly patients often seek care because of back and leg pain that may be caused by scoliosis and associated spinal stenosis.
According to 2010 US Census Population Estimate, there were 235,205,658 people in the United States over the age of 18 years. Prevalence of adult scoliosis cited in the literature ranges from 2.5% to 60%, depending on severity. A conservative estimate (2.5%) of the prevalence of adult scoliosis yields an incidence of a minimum of 5.88 million adults in the United States with adult scoliosis. In 2013, an estimated 1.28 million of these adults received treatment either as an inpatient or on an outpatient basis. (Reference Table 2B.2.2 PDF [18] CSV [19])
The management of adult scoliosis includes nonsurgical and surgical resources. Nonsurgical treatments of adult scoliosis utilize significant resources, and include interventions such as exercises, physical therapy, injections, pain medications, and manual manipulation.9 Data on nonsurgical treatments is not available; however, a 2010 nonrandomized study reported that two years of nonsurgical treatment in adult scoliosis patients resulted in substantial expenditures and yielded no improvement in health status.10
Operative management of scoliosis in the adult encompasses a spectrum of procedures, including decompression alone, decompression with limited fusion, and fusion of the deformity. The type of procedure performed is typically determined by the predominant symptoms. Neural symptoms in patients with smaller curves (<30 degrees) are treated with decompression alone, while patients with larger curves and neural symptoms are treated with decompression and fusion.11 Adult scoliosis associated with sagittal deformity is more commonly treated with decompression, osteotomies, and larger fusions of greater than four level (five or more vertebrae).12
In 2013, a query of the Healthcare Costs and Utilization Project (HCUP) Nationwide Inpatient Survey (NIS) resulted in approximately 142,600 hospitalizations of people age 18 and over associated with a discharge diagnosis of scoliosis (ICD-9-CM of 373). The majority of these, or 140,200 patients, were diagnosed as idiopathic scoliosis or scoliosis of unknown cause. Hospitalization with a scoliosis diagnosis was higher among the elderly, with those 65 and older accounting for nearly half (43%) among all ages. Females accounted for nearly three-quarters (73%) of all scoliosis hospitalizations. Race/ethnicity and region in the US did not show significant differences. (Reference Table 2B.2.1 PDF [5] CSV [6], Table 2B.2.2 PDF [18] CSV [19], Table 2B.2.3 PDF [36] CSV, [37] Table 2B.2.4 PDF [38] CSV [39])
In 2013, more than one-half (53.6%) of patients with a diagnosis of acquired/secondary scoliosis had a surgical procedure, but only one in five (20.7%) of those with a diagnosis of idiopathic scoliosis had surgery. The most common procedure performed on scoliosis patients was spinal fusion, with 26,600, or 16%, having this procedure. A majority of scoliosis patients with a fusion procedure (83%) had fusion of 4 or more levels. Sex of the patient was not a factor in having a procedure, but persons age 45 to 64 were most likely to have a procedure. (Reference Table 2B.5.0.1 PDF [40] CSV [41], Table 2B.5.0.2 PDF [42] CSV [43], Table 2B.5.1 PDF [44] CSV [45], Table 2B.5.2 PDF [22] CSV [23])
The cost of care for adults with scoliosis includes direct costs and indirect costs of lost wages, time away from work, cost of care providers, and opportunity costs. Estimates of the direct costs of nonsurgical care in adult scoliosis are estimated to be as high as $14,000 per year.10 The national mean cost of a hospitalization, including surgical treatment, for patients with a primary diagnosis of idiopathic scoliosis was $69,400 in 2013 for an average hospital stay of 5.3 days. The mean cost for those with an acquired or secondary scoliosis diagnosis were significantly higher at $120,400 per discharge, with an average stay of 5.9 days. The HCUP NIS database does not provide hospitalization costs associated with secondary discharge diagnoses, and does not include fees to doctors, tests, and other typical charges associated with hospitalization. Therefore, the most conservative estimate of only the hospitalization cost for adult scoliosis, both idiopathic and acquired/secondary in 2013 was an estimated $11.5 billion (166,600 hospitalizations). Charges are not necessarily actual costs paid. Mean charges for scoliosis diagnosed patients are significantly higher than for all hospital discharge patients. (Reference Table 2B.3.2 PDF [26] CSV [27])
In 2013, slightly more than one-half (58%) of patients with a scoliosis diagnosis were discharged to home, while 70% of patients with any diagnosis had a routine discharge. Patients with a scoliosis diagnosis are more likely to be transferred to a skilled nursing or intermediate care facility (long-term care) than are patients with all diagnoses. This is particularly true for the elderly population, with 39% of persons age 65 and older with a scoliosis diagnosis moving to a long-term care facility. (Reference Table 2B.4.2 PDF [32] CSV [33])
The real cost of the management of adult scoliosis to our healthcare system is significant, and the value of care measured by change in health status remains incompletely defined for both nonsurgical and surgical care.
Recent emphasis has been placed on sagittal plane balance and restoring normal sagittal alignment with regards to the three dimensional deformity of adult spinal deformity (ASD), and is a primary condition leading to the high prevalence (68%) of persons age 60 and over with adult spinal deformity.1,2 The impact of sagittal plane alignment on the treatment of spinal disorders is of critical importance. A failure to recognize malalignment in this plane can have significant consequences for the patient not only for pain and deformity, but also social interaction due to deficient forward gaze. A good understanding of the principles of sagittal balance is vital to achieve optimum outcomes when treating spinal disorders. Even when addressing problems in the coronal plane (front from back), an awareness of sagittal balance is necessary to avoid future complications.3
Sagittal plane deformity presents as an exaggeration or deficiency of normal lumbar lordosis (inward curving of the lumbar spine just above the buttocks) or kyphosis (exaggerated curvature of the upper (thoracic) spine). There are variations on the degree of normal curvature, still this shape allows equal distribution of forces across the spinal column. It is the disruption of this equilibrium by pathological processes or, as in most cases, ageing that results in deformity. This leads to adaptive changes in the pelvis and lower limbs. The effects of limb alignment on spinal posture are well documented. Changes in pelvic posture also affect spinal alignment.3
A lordosis deformity is usually iatrogenic (illness or condition caused by medication or treatment), and often follows lumbar fusion, thoracolumbar fusion, and, in some cases, lumbar decompressive procedures. Nonsurgical causes include ankylosing spondylitis, degenerative changes, or adult presentation of adolescent idiopathic scoliosis. The deformity may lead to neurogenic radicular symptoms secondary to stenosis, paraspinal muscular fatigue, and low back pain. Nonoperative treatment options fail for most patients. Surgical interventions are aimed at restoring lumbar lordosis, which is typically accomplished with revision decompression, fusion, and various osteotomies.4
Kyphosis is often secondary to inflammatory, degenerative, or post- traumatic disorders, and can be caused by poor posture, slouching, osteoporosis, birth defects, or disease. They may also be secondary to infection or tumors. There is usually pain and functional disability along with concerns about self-image and social interaction due to inability to maintain a horizontal gaze. The resultant pelvic and lower limb posture is an attempt to restore normal alignment. Addressing this complex problem requires detailed expertise and awareness of the potential pitfalls surrounding its treatment.1
Increasingly positive sagittal imbalance has been shown to correlate with poor functional outcome and poor self-image along with poor psychological function. Restoring normal spinopelvic alignment is paramount to the treatment of complex spinal deformity with sagittal imbalance. Understanding of whole spinal alignment and dynamics of spinopelvic alignment is essential to restore sagittal balance while minimizing the risk of developing sagittal decompensation after surgical intervention.1,3
The goal of sagittal deformity management is to maintain the body in an energy-efficient, ergonomically favorable erect position. The larger the deviation from a balanced alignment, the more energy an individual uses to stand upright without external suport. Patients with symptomatic sagittal plane deformity often present with a sagittal balance at the periphery of this balanced alignment, leading to an increased effort of accessory musculature to maintain the head over the pelvis. This leads to fatigue and pain, especially with prolonged activity. As sagittal imbalance progresses, different compensatory mechanisms such as the pelvic retroversion, hip extension, and knee flexion are used in order to restore and maintain sagittal balance. Once a spinal deformity surpasses these compensatory mechanisms surgical intervention is often requested.5
Operative management of sagittal deformity in the adult encompasses a spectrum of procedures with fusion the most common. In 2013, a query of the Healthcare Costs and Utilization Project (HCUP) Nationwide Inpatient Survey (NIS) resulted in approximately 190,500 hospitalizations associated with a discharge diagnosis of sagittal deformity. The largest share (76%), or 144,600 patients, were diagnosed with spondylolisthesis. Hospitalization with a sagittal deformity diagnosis was higher among the elderly, accounting for more than one-half (54%) among all ages for those 65 and older. Females accounted for 69% of all sagittal deformity hospitalizations. Race/ethnicity and region in the US did not show significant differences. (Reference Table 2B.2.1 PDF [5] CSV [6], Table 2B.2.2 PDF [18] CSV [19], Table 2B.2.3 PDF [36] CSV [37], Table 2B.2.4 PDF [38] CSV [39])
In 2013, more than nearly three-fourths (72.3%) of patients with a diagnosis of sagittal deformity had a surgical procedure. A diagnosis of spondylolisthesis had the highest rate (84.6%) of surgical procedure. The most common procedure performed on sagittal deformity patients was spinal fusion, with 67.4%, having this procedure. More than one-half (56%) had fusion of less than four levels. Sex of the patient was not a factor in having a procedure, but persons age 45 to 64 were most likely to have a procedure. (Reference Table 2B.5.0.1 PDF [40] CSV [41], Table 2B.5.0.2 PDF [42] CSV [43], Table 2B.5.1 PDF [44] CSV [45], Table 2B.5.2 PDF [22] CSV [23])
Sagittal balance is an independent predictor of clinical outcomes in spinal care. Surgical treatment is challenging and jeopardized by frequent complications. Guidelines for surgical treatment are currently not based on a classification of the disease. A comprehensive classification of sagittal balance based on regional deformities and compensatory mechanisms combined in deformity patterns is proposed. Though the sagittal shape of the spine can change due to degeneration or trauma, correlations between sagittal shape parameters and pelvic incidence (PI) have been described. PI is not changed by degeneration, thus representing a permanent source of information on the original sagittal shape of the spine.6
The national mean cost of a hospitalization, including surgical treatment, for patients with a primary diagnosis of sagittal imbalance was $94,500 in 2013 for an average hospital stay of 4.3 days. The HCUP NIS database does not provide hospitalization costs associated with secondary discharge diagnoses, and does not include fees to doctors, tests, and other typical charges associated with hospitalization. Therefore, the most conservative estimate of only hospital charges for adult sagittal imbalance in 2013 was an estimated $18.0 billion (166,600 hospitalizations). Charges are not necessarily actual costs paid. Mean charges for sagittal imbalance diagnosed patients are significantly higher than for all hospital discharge patients. (Reference Table 2B.3.2 PDF [26] CSV [27])
In 2013, slightly more one-half (56%) of patients with a sagittal imbalance diagnosis were discharged to home, compared to 70% of patients with any diagnosis. Patients with a sagittal imbalance diagnosis are more likely to be transferred to a skilled nursing or intermediate care facility (long-term care) than are patients with all other diagnoses. This is particularly true for the elderly population, with 36% of persons age 65 and older with a sagittal imbalance diagnosis moving to a long-term care facility. (Reference Table 2B.4.2 PDF [32] CSV [33])
The real cost of the management of adult sagittal imbalance to our healthcare system is significant, and the value of care measured by change in health status remains incompletely defined for both nonsurgical and surgical care.
Spinal deformity can be caused by congenital conditions and due to aging wear and tear on the back. Medical conditions and poor bone quality may also contribute to spinal deformity, however, in many cases the cause remains unknown.
Several conditions known to contribute to spinal deformity were examined as cross diagnoses with spinal deformity at the time of a healthcare visit. The most frequent diagnosis with one in ten (9.3%) hospital discharges and a scoliosis diagnosis was congenital spinal disorders. Four other conditions – trauma/spinal fractures, spinal infections, spondylopathies, and complications of surgery – were found in less than 2% of scoliosis and between 2% and 4% of sagittal imbalance hospital discharge diagnoses. Looking at all healthcare resources, the cross-diagnosis of spinal deformity and a contributing cause dropped to 0.3% among scoliosis discharges and 0.2% among sagittal imbalance visits. (Reference Table 2B.6.0 PDF [62] CSV [63])
Several studies have examined the relationship between spinal deformity and contributing causes, but until identification of multiple conditions is made, no clear relationship can be established.
The burden of spinal deformity includes healthcare costs, pain management, therapy, alternative care, and lost workdays due to pain. The total cost of spinal deformity is difficult to determine because hospital charges are the only expenditures available in the databases. In addition, not all persons suffering from spinal deformity seek medical care.
In 2013, charges for 357,000 hospital discharges for spinal deformity were $29.5 billion. Spinal deformity charges accounted for 2.1% of all hospital charges in 2013, but only 1% of hospital discharges. (Reference Table 2B.3.1 PDF [66] CSV [67])
In addition to direct and indirect costs, persons afflicted with spinal deformity experience a reduced quality of life, which may include major constraints on mobility and activity for those with the most serious conditions.
While technical outcomes of surgery are well known and show obvious benefits for those with significant deformity, long-term health related outcomes have yet to be precisely documented. The lack of quality, long-term studies of sufficient size hampers our understanding of the mortality and morbidity rates for patients with congenital and idiopathic scoliosis, with and without treatment. Fifty years of follow-up studies of children and adolescents with untreated scoliosis have shown conflicting results, with some studies indicating a higher risk of mortality and respiratory compromise.1,2
Another study shows compromise only in patients with early reduced lung function and a large curvature.3 Yet another study has shown no differences in untreated childhood scoliosis and a control group.4 Several articles from the 1960s and one recent article report that low back pain does not occur more frequently in untreated scoliosis patients than in the general population4,5,6 unless the curvature is greater than 40°.7,8 It has also been shown that persons treated with surgery rather than bracing for adolescent idiopathic scoliosis have less pain at 10- to 20-year follow-up, although function remains similar.9,10 The cosmetic/self-image aspect of scoliosis is obvious and important, and often a major factor affecting the lives of individuals with this condition.
Scoliosis in the adult has an impact that is similar to other common medical conditions including osteoarthritis, coronary artery disease, and chronic obstructive pulmonary disease. Overall, the burden of scoliosis on health-related quality of life is severe relative to other common medical conditions. With the aging demographic profile of the US, the burden of adult scoliosis is increasing and has a significant impact on the health of our population, and on the cost of care for spinal disorders.
Likewise, vertebral compression fractures, which may contribute to adult degenerative scoliosis, are also a growing concern for the aging population, particularly when associated with kyphosis and/or disabling pain.
With the sagittal profile of the spine, conventional thinking has been to categorize it into different segments based on the anatomical differentiation of the vertebrae. This delineation does not take into account the true surface contour of the spine. The disadvantage of this overly simplistic categorization is that when attempting to restore what is perceived as a ‘normal thoracolumbar spine,’ a ‘one size fits all’ approach is used.1
Increased understanding of sagittal plane deformity will lead to earlier identification. As the life expectancy of the population increases along with the patients desire to lead more active lives well into advanced years, so will the demand for appropriate expertise and skill in dealing with this complex problem. Spinal osteotomies remain complicated procedures. This treatment strategy must be the subject of specific training and must be practiced by specialist surgeons for the best outcomes.1
Curvature of Spine:
Idiopathic Scoliosis: 737.30-737.32
Acquired Kyphosis and Lordosis: 737.0, 737.10, 737.12, 737.19, 737.20-737.29, 737.34, 737.39
Secondary Scoliosis, Kyphosis, and Lordosis: 737.11, 737.33, 737.40-737.43, 737.8, 737.9
Spondylolisthesis: 737.40, 756.12
Adolescent Postural Kyphosis: 737.00
Kyphosis: 737.10-737.19, 737.41
Lordosis: 737.20-737.29, 737.42
Scoliosis: 737.30-737.39, 737.40, 737.43, 737.8, 737.9
Trauma: Spinal Fractures Contributing to Deformity:
Vertebral Compression Fractures: 805.00-805.08, 805.2, 805.4, 805.6, 805.8
Traumatic Fractures: 805.10-805.18, 805.3, 805.5, 805.7, 805.9, 806.00-806.09, 806.10-806.19, 806.20-806.29,806.30-806.39, 806.4, 806.5, 806.60-806.02, 806.69, 806.70-806.72, 806.79, 806.8, 806.9
Infection/Complications Codes:
Tuberculosis of Vertical Column: 015.00 to 015.06
Tuberculosis Unspecified: 015.90 to 015.96
Intracranial and Intraspinal Abscess (Epidural abscess): 324.1, 324.9
Acute Osteomyelitis: 730.00, 730.08, 730.09
Chronic Osteomyelitis: 730.10, 730.18, 730.19
Discitis: 722.90 to 722.93
Complications of Surgery: 996.2, 996.59, 996.63, 996.72
Spondylopathies:
Ankylosing Spondylitis: 720.00
Spinal Enthesopathy: 720.1
Sacroiliitis, not elsewhere classified: 720.2
Other Inflammatory Spondylopathies: 720.81, 820.89
Unspecified Inflammatory Spondylopathy: 720.9
Cervical Spondylosis with Myelopathy: 721.1
Thoracic or Lumbar Spondylosis with Myelopathy: 721.4
Spondylosis with Myelopathy, Thoracic Region: 721.41
Spondylosis with Myelopathy, Lumbar Region: 721.42
Intervertebral Disc Disorder with Myelopathy: 722.70 to 722.73
Spinal Stenosis in Cervical Region: 723.00
Cervicalgia: 723.1
Cervicocranial Syndrome: 723.2
Cervicobrachial Syndrome (diffuse): 723.3
Brachial Neuritis or Radiculitis NOS: 723.4
Torticollis, Unspecified: 723.5
Panniculitis Specified as Affecting Neck: 723.6
Ossification of Posterior Longitudinal Ligament in Cervical Region: 723.7
Spinal Deformity Procedures:
Decompression: 0309, 8050, 8051
Cervical Fusion: 8102, 8103
Thoracic/Dorsal or Dorsolumbar Fusion: 8104, 8105
Lumbar and Lumbosacral Fusion: 8106, 8107, 8108
Other Fusion: 8100, 8101
Cervical Refusion: 8132, 8133
Thoracic, Dorsal or Dorsolumbar Refusion: 8134, 8135
Lumbar and Lumbosacral Refusion: 8136, 8137, 8138
Other Refusion: 8130, 8131, 8139
Fusion/Refusion of Multiple Vertebrae: 8162, 8163, 8164
Instrumentation/Insertion of Spinal Device: 8451, 8452, 8459
Vertebraplasty: 8165
Kyphoplasty [Percutaneous Vertebral Augmentation]: 8166 Decompression: 0309
Diskectomy: 8050, 8051
Epidural injection: 8192, 8396, 8397
Links:
[1] https://bmus.latticegroup.com/docs/bmus_e4_T2B.1.0.pdf
[2] https://bmus.latticegroup.com/docs/bmus_e4_T2B.1.0.csv
[3] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.0.pdf
[4] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.0.csv
[5] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.1.pdf
[6] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.1.csv
[7] https://bmus.latticegroup.com/file/bmuse4g2b210png
[8] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.0.png
[9] https://bmus.latticegroup.com/file/cobb-anglepng
[10] https://bmus.latticegroup.com/docs/cobb-angle.png
[11] https://bmus.latticegroup.com/file/adolescent-prevalencepng
[12] https://bmus.latticegroup.com/docs/adolescent%20prevalence.png
[13] https://bmus.latticegroup.com/file/congenital-scoliosis-syndromespng
[14] https://bmus.latticegroup.com/docs/congenital%20scoliosis%20syndromes.png
[15] https://www.srs.org/patients-and-families/conditions-and-treatments/parents/scoliosis
[16] http://www.ncbi.nlm.nih.gov/pubmed/15931035
[17] http://www.wheelessonline.com/ortho/congenital_scoliosis_and_vertebral_defects
[18] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.2.pdf
[19] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.2.csv
[20] https://bmus.latticegroup.com/file/bmuse4g2b211png
[21] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.1.png
[22] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.2.pdf
[23] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.2.csv
[24] https://bmus.latticegroup.com/file/bmuse4g2b212png
[25] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.2.png
[26] https://bmus.latticegroup.com/docs/bmus_e4_T2B.3.2.pdf
[27] https://bmus.latticegroup.com/docs/bmus_e4_T2B.3.2.csv
[28] https://bmus.latticegroup.com/file/bmuse4g2b213png
[29] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.3.png
[30] https://bmus.latticegroup.com/file/bmuse4g2b214png
[31] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.1.4.png
[32] https://bmus.latticegroup.com/docs/bmus_e4_T2B.4.2.pdf
[33] https://bmus.latticegroup.com/docs/bmus_e4_T2B.4.2.csv
[34] https://bmus.latticegroup.com/file/bmuse4g2b221png
[35] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.2.1.png
[36] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.3.pdf
[37] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.3.csv
[38] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.4.pdf
[39] https://bmus.latticegroup.com/docs/bmus_e4_T2B.2.4.csv
[40] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.0.1.pdf
[41] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.0.1.csv
[42] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.0.2.pdf
[43] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.0.2.csv
[44] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.1.pdf
[45] https://bmus.latticegroup.com/docs/bmus_e4_T2B.5.1.csv
[46] https://bmus.latticegroup.com/file/bmuse4g2b222png
[47] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.2.2.png
[48] https://bmus.latticegroup.com/file/bmuse4g2b223png
[49] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.2.3.png
[50] https://bmus.latticegroup.com/file/bmuse4g2b224png
[51] https://bmus.latticegroup.com/docs/bmus_e4_g2b.2.2.4.png
[52] https://bmus.latticegroup.com/file/sagittal-plane-deformitypng
[53] https://bmus.latticegroup.com/docs/sagittal%20plane%20deformity.png
[54] https://bmus.latticegroup.com/file/bmuse4g2b31png
[55] https://bmus.latticegroup.com/docs/bmus_e4_g2b.3.1.png
[56] https://bmus.latticegroup.com/file/bmuse4g2b32png
[57] https://bmus.latticegroup.com/docs/bmus_e4_g2b.3.2.png
[58] https://bmus.latticegroup.com/file/bmuse4g2b33png
[59] https://bmus.latticegroup.com/docs/bmus_e4_g2b.3.3.png
[60] https://bmus.latticegroup.com/file/bmuse4g2b34png
[61] https://bmus.latticegroup.com/docs/bmus_e4_g2b.3.4.png
[62] https://bmus.latticegroup.com/docs/bmus_e4_T2B.6.0.pdf
[63] https://bmus.latticegroup.com/docs/bmus_e4_T2B.6.0.csv
[64] https://bmus.latticegroup.com/file/bmuse4g2b41png
[65] https://bmus.latticegroup.com/docs/bmus_e4_g2b.4.1.png
[66] https://bmus.latticegroup.com/docs/bmus_e4_T2B.3.1.pdf
[67] https://bmus.latticegroup.com/docs/bmus_e4_T2B.3.1.csv