 [5]
[5] 

Sports are integrally woven into the fabric of American society. From being a fan, through participation in recreational athletics, all the way to participation in competitive club, high school, collegiate, and professional athletics, sports are an important facet of our lives. Participation in sports and physical activities have several noted health and psychological benefits; however, over the past few decades, an increase in participation in both youth sports as well as recreational activity has been noted – with a resultant increase in both acute and chronic musculoskeletal injuries.
The goal of this section is to provide an overview of the epidemiology of athletic injuries in the United States population. As we ascend the athletic ladder from recreational activities to professional sports, we note an increase in participation and injury data available. However, we have poor mechanisms and infrastructure to study injuries among those engaged in the lowest levels of athletic participation. For example, there is limited data on the middle-aged person who begins jogging for fitness or the 12-year old who rides a bicycle. Similarly, as youth sports club participation has become more popular in the United States there are few resources to study injuries in this setting. We will attempt to provide an overview of these less organized athletic injuries from available data. We will also focus on higher levels of organized sports, primarily scholastic sports (high school level) and intercollegiate sports.
It is estimated that 30 million children and adolescents participate in organized sports. In addition, some 150 million adults participate in physical activity and recreational activities that are not related to their employment.1 However, both these large at-risk populations lack a systematic mechanism for tracking musculoskeletal injuries and conditions.
While professional, collegiate, and even high school athletics have epidemiologic systems in place to track injury patterns, recreational athletics lack any type of surveillance system. However, the US Consumer Product Safety Commission established the National Electronic Injury Surveillance System [1] (NEISS) in 1997 to track emergency room visits and injury patterns associated with specific products. This database has also been helpful as a means of documenting injuries associated with athletic, physical activity, and recreational endeavors. However, a major limitation of this data is that injuries not significant enough to require an emergency room visit, or injuries that are seen in other healthcare settings (e.g., athletic training room, primary care clinic, specialty clinic) may not be documented and reported. Regardless, the NEISS probably provides the best available nationwide estimates on recreation related and physical activity injuries significant enough to require an emergency room visit.
Using the data from the NEISS, a 2002 CDC report detailed 4.3 million sports and recreation related injuries that were treated in US emergency departments.1 The injury rate was highest for boys ages 10-14. A more recent paper documented that an estimated 600,000 knee injuries present annually to emergency rooms in the United States. Of these, 49.3% resulted from participating in sports and recreation activities.2
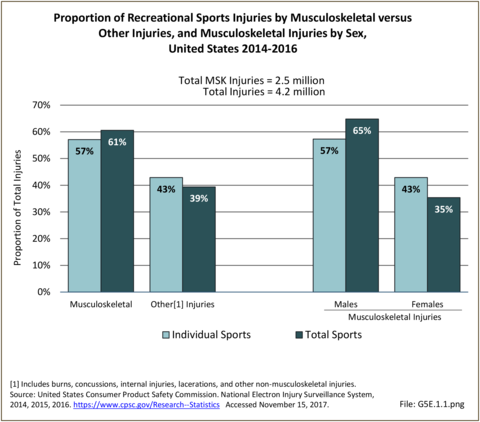
More recent data from the NEISS for the years 2014 through 2016 reveal similar patterns. During this time period a total of 4.2 million emergency room visits were documented for injuries related to sports participation, physical activity, and recreational endeavors. Of those, 1.5 million were due to participation in team sports and 2.8 million injuries resulted from individual sports and recreational activities, of which 61% impacted the musculoskeletal system. Two out of three musculoskeletal injuries occur to males, with the proportion lower for individual sports (57%) than for team sports (77%). Of the estimated 2.8 million injuries resulting from individual sports that present annually to emergency rooms in the US, 57% impact the musculoskeletal system. Two out of three musculoskeletal injuries (65%) occur to males, with the proportion being slightly smaller among males for individual sports than for team sports. (Reference Table 5E.1.1 PDF [2] CSV [3])
Cycling and wheeled sports account for 19.9% of all recreational sports injuries and musculoskeletal injuries serious enough to warrant a visit to the ED. Fitness training results in an additional 16.3% of the total number of musculoskeletal injuries seen. Musculoskeletal injuries account for more than 50 percent of all injuries in all sports, with the exception of water sports. (Reference Table 5E.1.1 PDF [2] CSV [3])
Musculoskeletal injuries treated in the ED as a result of a recreational sport injury occur in the highest proportion in kids ages 2 through 18. According to the latest data, nearly 60% of all musculoskeletal injuries due to participating in individual and team sports and recreational activities occur in this age range. This is, in part, due to the high number of playground injuries, as well as biking and other wheeled equipment, such as skateboards and scooters, but kids account for a higher proportion of treated sports injuries in all but a few sports that are more adult focused. Adults between the ages of 19 and 44 also account for a substantial proportion (29%) of treated musculoskeletal injuries, but they are also a larger share of the population and more likely to be active in recreational sport activities. (Reference Table 5E.1.2.1 PDF [8] CSV [9])
Sprains and strains, primarily affecting the joints and muscles, are the most common reason for seeking care in the emergency department for sports and physical activity related injuries. An estimated 41.2% of musculoskeletal injuries seen in emergency departments due to participating in recreational sports and physical activities result in sprains or strains, followed by bone fractures (30.4%), contusions (24.3%), and joint dislocations (3.8%). (Reference Table 5E.1.3 PDF [12] CSV [13])
Injuries from team and individual sports to the extremities are the most common, with 41.3% occurring in the upper extremity compared with 37.5% in the lower extremity. The trunk sustains most of the remaining injuries (14.4%), with less than 6% involving the head, although head injuries are often unreported. (Reference Table 5E.1.4 PDF CSV) Among team sports, kids age 2 to 12 are the most likely to injure the upper extremity in all except those playing hockey, where participation numbers in this age range are low. (Reference Table 5E.1.7 PDF [16] CSV [17])
Nearly all (96%) musculoskeletal injuries due to sports and recreational activities seen in the ED are treated and released. This compares to just over 81% for all emergency department visits. Only 3% of recreational activity and sports injuries seen in EDs result in hospitalization. Among individual sports, 4.1% of musculoskeletal injuries seen in the ED resulted in hospitalization with the highest proportion of injuries from mountain climbing (12.1%), all-terrain vehicles and motorized bikes (8.1%), and bicycle/wheeled activities (bicycles, skateboards, scooters, etc.) (6.1%). Among team sports only 1.1% of injuries seen in the ED resulted in hospitalization, with the highest proportion reported in soccer (1.5%), followed by hockey (1.4%) and football (1.3%). (Reference Table 5E.1.5 PDF [20] CSV [21])
It is not surprising that the majority of injuries treated in emergency departments due to sports participation and recreational physical activities occur on sports fields (37.5%), with 50.9% of team sports injuries and 29.2% of individual sports injuries occurring in this setting. (Reference Table 5E.1.6 PDF [24] CSV [25])
Scholastic sports have nearly doubled from an estimated 4.0 million participants in 1971-1972 1 to 7.98 million participants in 2017-2018.2 These high school athletes experienced an estimated 1.4 million injuries in 2017-2018.3 Data from the National High School Sports-Related Injury Surveillance System [28] using RIO (Reporting Information Online) as a surveillance system, was used to examine injury rates and trends. This data provides quality epidemiologic information entered by athletic trainers associated with participating high schools and provides nationwide estimates for injury incidence rates in common high school sports.
Using the National High School Sports-Related Injury Surveillance Study, it was estimated that more than 17 million injuries resulted from participation in team sports at the high school level during the 13 years studied between the 2005-2006 and 2017-2018 school years. On average, of the total injuries documented during the surveillance period, strains/sprains accounted for 44%, concussions represented 18%, contusions comprised 11%, and fractures were documented in 9% of cases. Injuries categorized as “other” comprised 18% of all injuries. Overall, the majority of injuries from participating in high school athletics impacted the musculoskeletal system.4
Football had the highest injury incidence rate for musculoskeletal injuries among all team sports at the high school level, followed by girls’ soccer and boys’ wrestling. In 2017-2018, football also had the greatest number of total injuries as well. In every sport besides girls’ volleyball and boys’ wrestling, more injuries occurred during competition when compared to practice.
Musculoskeletal injuries occur at numerous different sites throughout the body. On average, between 2012 and 2018, 21% of all injuries were to the head/face, 17.5% impacted the ankle, 14.5% occurred in the knee, 9.5% affected the hip/thigh/upper leg, 7.5% affected the shoulder, 8% were to the hand/wrist, 5% to the trunk, 5% to the lower leg, 4% to the arm/elbow, 4% affected the foot, and 2% of all injuries were to the neck. Injuries categorized as “other” comprised 2% of all injures. The ankle and knee, two of the most injured joints accounted for a combined total of 32% of all musculoskeletal injuries among high school athletes.5 This is consistent with the most recent data available for the 2017-18 academic year.6
Musculoskeletal injuries also account for substantial time loss from playing a sport. On average, between 2012 and 2018, 17% of all injuries resulted in 1-2 days of time loss; 24% resulted in 3-6 days of time loss; 16% resulted in 7-9 days of time loss; 19% resulted in 10-21 days of time loss; and 23% resulted in greater than 21 days of time loss or medical disqualification for the season, medical disqualification for the career, or an injury that did not resolve prior to the end of the season permitting return to play. One in four (24%) resulted in 3-6 days of time loss, which can equate to missing an entire week of practice and games, but nearly as many (23%) injuries resulted in missing 22 or more days or not returning to sport during the same season.7 During the same time period, between 5.3% and 8.2% of injuries annually required surgical intervention to repair.8
Though nearly 95% of all sports-related injuries seen in emergency departments are treated and released, as noted in the discussion of recreational athletics above, emergency medical system (EMS) transport among high school athletes is relatively uncommon. The overall rate of EMS transport among high school athletes participating in organized sports is 0.29 transports per 10,000 athlete exposures, according to a recent report.9 Nearly 60% of the injuries requiring EMS transport impacted the musculoskeletal system, with the most common injuries including fractures (24%), strains (12%), dislocations (11%), and sprains (10.3%).
Trends in annual injury incidence rates for high school athletes over time are presented in Graphs 5E.2.3a thru 5E.2.3h and the total annual number of injuries among high school athletes over time based on the RIO data are presented in Graph 5E.2.4. Overall, these data have remained relatively stable between 2005-2006 and 2017-2018. Annual incidence rates over time for specific high school sports during this time period are also presented. Some significant trends have been reported.10 Specifically, there have been statistically significant decreases in the annual injury incidence rate for boys’ high school soccer and basketball during practice sessions; however, there has also been a significant increase in the annual incidence rate for girls’ high school soccer in competitions.
While less data is available on long term health impacts of musculoskeletal injuries in scholastic athletes, one such study by McLeod and colleagues offers insight into the significant impact of athletic injury in this large population.11 The research team studied a convenience sample of 160 uninjured and 45 injured scholastic athletes with health-related quality of life measures. They found significantly lower scores among the injured athletes for the following subscores of the Quality of Life Short Form Questionnaire (SF-36):12 physical functioning, limitations due to health problems, bodily pain, social functioning, and the physical composite score. These findings suggest that physical injuries in our young athletes affect not only their physical function and risk for future musculoskeletal injury and disability, but also extend beyond the physical aspects of overall health. Limited data is available on the long-term health related impact of musculoskeletal injuries experienced by high school athletes.
The National Collegiate Athletic Association [58] (NCAA) is a non-profit association that regulates athletes of more than 1,200 institutions, conferences, organizations, and individuals that organize athletic programs of many colleges and universities in the United States and Canada. Athletic programs of more than 1,100 member schools that compete are divided into three levels or divisions.1 Nearly a half-million student-athletes participate in NCAA sports that offer national championships annually, and this number continues to grow. During the 2018-2019 academic year, the number of teams competing in NCAA championship sponsored sports reached an all-time high of 19,750. However, only about 6% of high school athletes will participate in NCAA intercollegiate sports.2
While there are numerous benefits associated with participating in collegiate athletics, there is also an increased risk of injury associated with participating in many types of sports. These injuries primarily affect the musculoskeletal system, in general, and the lower and upper extremities specifically. Though awareness of risk of injury associated with participating in collegiate athletics is growing, there is little known about the long-term impact of injuries sustained while participating in collegiate athletics. Recent injury data from the NCAA Injury Surveillance System [59], as well as reports for specific joint injuries sustained by NCAA athletes and emerging data on the potential long-term impact of these injuries on health related quality of life, is presented.
For over 30 years, the NCAA and the Datalys Center [60] (since 2009) has been engaged in active injury surveillance within the unique population of college athletes. Collaborative efforts between the NCAA and the National Athletic Trainers’ Association [61] (NATA) have yielded rich injury surveillance data used to inform important rule changes to protect player safety.3 In a 2007 special issue of The Journal of Athletic Training, data from the NCAA injury surveillance system from the 1988-89 academic year through the 2003-2004 academic year were reviewed for 15 collegiate sports.4 With permission from the publisher, data from this study is included in this site. To read the full article, click here [62].
The 15 sports examined included five fall sports (men’s football, women’s field hockey, men’s soccer, women’s soccer, and women’s volleyball), six winter sports (men’s basketball, women’s basketball, women’s gymnastics, men’s gymnastics, men’s ice hockey, and men’s wrestling), and five spring sports (men’s baseball, men’s football, women’s softball, men’s lacrosse, and women’s lacrosse). Data for men’s spring football were only included in the analysis of practice injuries. These data provided an overall summary of the NCAA data from the years 1988-1989 through 2003-2004, made recommendations for injury prevention initiatives, and provided insight into the burden of musculoskeletal injury experienced by collegiate athletes. Some of these data are highlighted in this section. More recently, a series of papers on the first decade of web-based injury surveillance in high school and collegiate athletes have been published.5,6,7,8,9,10,11 These data are also briefly integrated here, as appropriate, as they provide further insight into the incidence and burden of musculoskeletal injuries in collegiate athletes. Overall, musculoskeletal injuries to the upper and lower extremity account for approximately 80% of all injuries among NCAA athletes; however, injury patterns vary slightly by sport. The CDC, which estimates 2.6 million children ages 0 through 19 years are treated in emergency departments each year for sports and recreation related injuries12, provides tips on how to prevent sports-related injuries in their Protect the Ones You Love Initiative [63]. Other professional societies and associations such as the American Orthopaedic Society for Sports Medicine’s (AOSSM) At Your Own Risk [64]and Stop Sports Injuries [65], and the National Athletic Trainers Association (NATA) Position Statements [66] also provide recommendations for injury prevention.
Overall, incidence rates for the 15 sports examined range from a high of 35.9 per 1,000 game athlete-exposures for men’s football to a low of 1.9 for men’s practice basketball. Among men, the highest injury rates were observed in football, wrestling, soccer, and ice hockey. Among women, the highest injury rates were experienced in soccer, gymnastics, ice hockey, and field hockey. (Reference Table 5E.3.2 PDF [67] CSV [68])
The majority of injuries resulted from contact with another player, regardless of whether or not injuries were sustained in practices or games. (Reference Table 5E.3.4 PDF [77] CSV [78])
The majority of injuries documented during the study period affected the musculoskeletal system, with 72% of all injuries in games and 75% of all injuries in practices affecting the extremities. Regardless of whether injuries occurred in practices or games, over half of all injuries reported across the 15 sports examined during the study period were to the lower extremity. (Reference Table 5E.3.5 PDF [81] CSV [82])
The NCAA injury surveillance system has also been used to examine the incidence and injury patterns of specific injuries among collegiate athletes.13,14These studies have primarily focused on those injuries that likely have the greatest burden in terms of time loss from sport, the need for surgical intervention, and the potential for long-term impact on health. Specifically, joint injuries have been a primary concern as it is well documented that these injuries can lead to chronic instability and increase the risk of osteoarthritis and degenerative joint disease.
Acute traumatic anterior cruciate ligament (ACL) injuries in the knee often lead to chronic pain and instability, and generally require surgical repair to restore function and stability. There is also substantial evidence to suggest that acute traumatic knee joint injuries such as ACL tears significantly increase the risk for post-traumatic osteoarthritis. Several studies have focused on the rate of ACL injuries among collegiate athletes.4,11,15,16,17 estimated that approximately 2,000 athletes participating in 15 different men’s and women’s NCAA sports sustain an ACL tear annually. The average annual rate of ACL injury during the 16-year study period examined was 0.15 per 1,000 athlete-exposures. Arendt and Dick16 first reported that there were disparities in ACL injury incidence rates between males and females participating in the NCAA gender matched sports of soccer and basketball. This observation was confirmed in a follow-up study that examined data from 1990 through 2002.15 The authors reported that the rate of ACL injuries was 3 times higher in female soccer players (0.33) when compared to male soccer players (0.11). Similarly, they reported that the rate of ACL injuries was 3.6 times higher in female basketball players (0.29) when compared to males (0.08). Regardless of sport, the rates in females were significantly higher when compared to males. They also reported that ACL injury rates declined significantly in male soccer players during the study period but remained constant among female soccer players. (Reference Table 5E.3.6 PDF [85] CSV [86])
Despite the decreases in ACL injury rates observed by Agel et al15 in male soccer players, Hootman et al4 reported that ACL injury rates among males and females combined, participating in 15 different NCAA sports, significantly increased during the 16-year study period. On average, they reported a 1.3% annual increase in the rate of ACL injury over time (P=0.02). (Reference Table 5E.3.7 PDF [73] CSV [74])
Dragoo et al13 compared ACL injury rates between NCAA football players participating on artificial turf and those participating on natural grass. They reported that the rate of ACL injury on artificial surfaces was significantly higher (1.39 times higher) than the injury rate on grass surfaces. A more recent study reports the injury rate on artificial turf 1.63 times higher than on grass surfaces.18 They also noted that non-contact injuries occurred more frequently on artificial turf surfaces (44%) than on natural grass (36%).
Ankle sprains are also common among NCAA athletes and they frequently lead to chronic pain, instability, and functional limitations. Hootman et al4 estimated that approximately 11,000 athletes participating in 15 different men’s and women’s NCAA sports sustain an ankle sprain annually. The average annual rate of ankle sprain injury during the 16-year study period examined was 0.86 per 1,000 athlete-exposures. They also examined the annual injury rates for ankle sprains among males and females participating in these sports combined between 1988 and 2004. They reported that injury rates remained constant during the 16-year study period. On average, there was a non-significant 0.1% (P=0.68) annual decrease in the rate of ankle sprains during the study period. (Reference Table 5E.3.6 PDF [85] CSV [86])
Shoulder injuries, especially those that result in instability, also impact a significant number of NCAA athletes and can lead to chronic pain, recurrent instability, and functional limitations. Recurrent shoulder instability has also been associated with the increased risk of osteoarthritis in the shoulder. Surgical reconstruction is common following shoulder instability in young athletes. Owens et al14 examined the injury rates and patterns for shoulder instability among NCAA athletes over the 16-year period from 1988 through 2004 in the same 15 sports described previously. The overall injury rate for shoulder instability during the study period was 0.12 per 1,000 athlete-exposures. On average, this is comparable to just under 2,000 shoulder instability events experienced annually in NCAA athletes. Injury rates for shoulder instability were significantly higher in games when compared to practice. Overall, NCAA athletes were 3.5 (95% CI: 3.29-3.73) times more likely to experience shoulder instability events in games when compared to practices. Just over half (53%) of the shoulder instability events documented during the study period were first time instability events, with the remaining injuries being recurrent instability events (47%). Most shoulder instability events were due to contact with another athlete (68%) and other contact (20%). Nearly half (45%) of all shoulder instability events experienced by NCAA athletes during the study period resulted at least 10 days of lost playing time, with the remainder returning to play within 10 days of injury.
While we still have a rudimentary understanding of the impact that musculoskeletal injuries sustained by collegiate athletes have on long-term health outcomes, studies have recently begun to examine health-related quality of life in current and former NCAA athletes. McAllister et al1 evaluated health-related quality of life in NCAA Division I athletes using the SF-362 and examined the association between scores, injury history and severity. Collegiate athletes who reported a history of mild injury had significantly lower physical component summary scale scores, role physical scores, bodily pain scores, social function scores, and general health scores on the SF-36 when compared to those with no history of injury. Collegiate athletes who reported a serious injury had significantly lower scores on all SF-36 component scores when compared to athletes with no history of injury. Similar results were observed in a separate study that examined NCAA Division I and Division II athletes.3
More recently, studies have examined health-related quality of life in former NCAA athletes. Sorenson et al4 reported that former NCAA Division I athletes were significantly more likely to have joint-related health concerns when compared to non-athletes and were 14 times more likely to seek professional treatment for their symptoms. They also reported that the prevalence of joint related health concerns was significantly higher in older former athletes when compared to younger former athletes.
In a similar study, Simon et al5 examined health-related quality of life in former NCAA Division I athletes and former non-athletes using the Patient-Reported Outcomes Measurement Information System (PROMIS).6 They reported that former collegiate athletes report significantly worse scores for 5 of the 7 PROMIS scales examined when compared to non-athletes. Specifically, former athletes reported poorer scores on the physical function, depression, fatigue, sleep disturbances, and pain interference scales. There were no differences noted between former NCAA athletes and non-athletes for the anxiety and satisfaction with participation in social roles scales. The authors also noted that former collegiate athletes reported significantly more major injuries, chronic injuries, daily limitations, and physical activity limitations when compared to non-athletes.
Overall, these studies suggest that NCAA athletes who sustain injuries during their college years have significantly lower health-related quality of life scores, and that these scores may get worse with time, particularly for joint-related health issues and long-term major and chronic injuries. Decreased health-related quality of life in former college athletes may also contribute to greater daily activity and physical activity limitations when compared to non-athletes and may lead to significant chronic health comorbidities. Further research is needed to determine which factors contribute to the poorer health-related quality of life outcomes observed among former collegiate athletes in these studies.
Links:
[1] https://www.cpsc.gov/Research--Statistics/NEISS-Injury-Data
[2] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.1.pdf
[3] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.1.csv
[4] https://bmus.latticegroup.com/file/bmus4eg5e11png
[5] https://bmus.latticegroup.com/docs/bmus_4e_g5e.1.1.png
[6] https://bmus.latticegroup.com/file/bmus4eg5e12png
[7] https://bmus.latticegroup.com/docs/bmus_4e_g5e.1.2.png
[8] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.2.1.pdf
[9] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.2.1.csv
[10] https://bmus.latticegroup.com/file/bmus4eg5e13png
[11] https://bmus.latticegroup.com/docs/bmus_4e_g5e.1.3.png
[12] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.3.pdf
[13] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.3.csv
[14] https://bmus.latticegroup.com/file/bmus4eg5e14png
[15] https://bmus.latticegroup.com/docs/bmus_4e_g5e.1.4.png
[16] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.7.pdf
[17] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.7.csv
[18] https://bmus.latticegroup.com/file/bmus4eg5e15png
[19] https://bmus.latticegroup.com/docs/bmus_4e_g5e.1.5.png
[20] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.5.pdf
[21] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.5.csv
[22] https://bmus.latticegroup.com/file/bmus4eg5e16png
[23] https://bmus.latticegroup.com/docs/bmus_4e_g5e.1.6.png
[24] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.6.pdf
[25] https://bmus.latticegroup.com/docs/bmus_4e_5e.1.6.csv
[26] https://bmus.latticegroup.com/file/bmus4eg5e17png
[27] https://bmus.latticegroup.com/docs/bmus_4e_g5e.1.7.png
[28] http://www.ucdenver.edu/academics/colleges/PublicHealth/research/ResearchProjects/piper/Pages/default.aspx
[29] https://bmus.latticegroup.com/file/bmus4eg5e21png
[30] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.1.png
[31] https://bmus.latticegroup.com/file/bmus4eg5e22png
[32] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.2.png
[33] https://bmus.latticegroup.com/file/bmus4eg5e23apng
[34] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3a.png
[35] https://bmus.latticegroup.com/file/bmus4eg5e23bpng
[36] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3b.png
[37] https://bmus.latticegroup.com/file/bmus4eg5e23c1png
[38] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3c1.png
[39] https://bmus.latticegroup.com/file/bmus4eg5e23c2png
[40] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3c2.png
[41] https://bmus.latticegroup.com/file/bmus4eg5e23dpng
[42] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3d.png
[43] https://bmus.latticegroup.com/file/bmus4eg5e23e1png
[44] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3e1.png
[45] https://bmus.latticegroup.com/file/bmus4eg5e23e2png
[46] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3e2.png
[47] https://bmus.latticegroup.com/file/bmus4eg5e23fpng
[48] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3f.png
[49] https://bmus.latticegroup.com/file/bmus4eg5e23gpng
[50] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3g.png
[51] https://bmus.latticegroup.com/file/bmus4eg5e23hpng
[52] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.3h.png
[53] https://bmus.latticegroup.com/file/bmus4eg5e24png
[54] https://bmus.latticegroup.com/docs/bmus_4e_g5e.2.4.png
[55] https://www.nfhs.org/articles/high-school-sports-participation-increases-for-29th-consecutive-year/
[56] http://www.ucdenver.edu
[57] http://www.ucdenver.edu/academics/colleges/PublicHealth/research/ResearchProjects/piper/projects/RIO/Documents/2017-18.pdf
[58] http://www.ncaa.org/
[59] http://www.ncaa.org/sport-science-institute/ncaa-injury-surveillance-program
[60] https://datalyscenter.org/index.php
[61] https://www.nata.org/
[62] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1941297/
[63] https://www.cdc.gov/safechild/nap/index.html
[64] https://www.atyourownrisk.org/
[65] https://www.stopsportsinjuries.org/
[66] https://www.nata.org/news-publications/pressroom/statements/position
[67] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.2.pdf
[68] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.2.csv
[69] https://bmus.latticegroup.com/file/bmus4eg5e31png
[70] https://bmus.latticegroup.com/docs/bmus_4e_g5e.3.1.png
[71] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.1.pdf
[72] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.1.csv
[73] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.7.pdf
[74] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.7.csv
[75] https://bmus.latticegroup.com/file/bmus4eg5e32png
[76] https://bmus.latticegroup.com/docs/bmus_4e_g5e.3.2.png
[77] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.4.pdf
[78] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.4.csv
[79] https://bmus.latticegroup.com/file/bmus4eg5e33png
[80] https://bmus.latticegroup.com/docs/bmus_4e_g5e.3.3.png
[81] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.5.pdf
[82] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.5.csv
[83] https://bmus.latticegroup.com/file/bmus4eg5e34png
[84] https://bmus.latticegroup.com/docs/bmus_4e_g5e.3.4.png
[85] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.6.pdf
[86] https://bmus.latticegroup.com/docs/bmus_4e_5e.3.6.csv
[87] https://bmus.latticegroup.com/file/bmus4eg5e35png
[88] https://bmus.latticegroup.com/docs/bmus_4e_g5e.3.5.png
[89] https://bmus.latticegroup.com/file/bmus4eg5e36png
[90] https://bmus.latticegroup.com/docs/bmus_4e_g5e.3.6.png
[91] https://bmus.latticegroup.com/file/bmus4eg5e37png
[92] https://bmus.latticegroup.com/docs/bmus_4e_g5e.3.7.png
[93] http://A: Estimated probability of competing in college athletics
[94] https://www.cdc.gov/safechild/sports_injuries/index.html