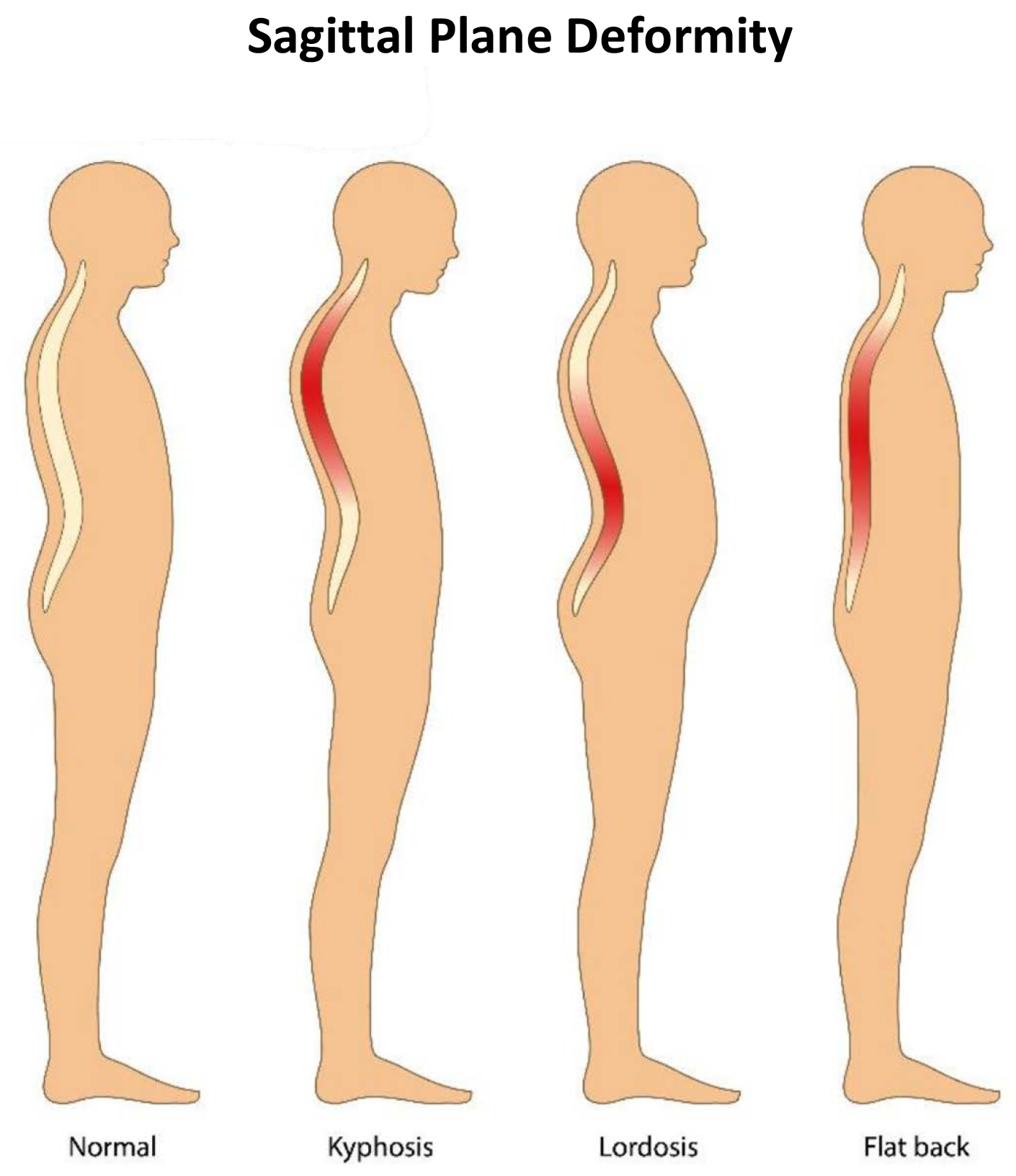
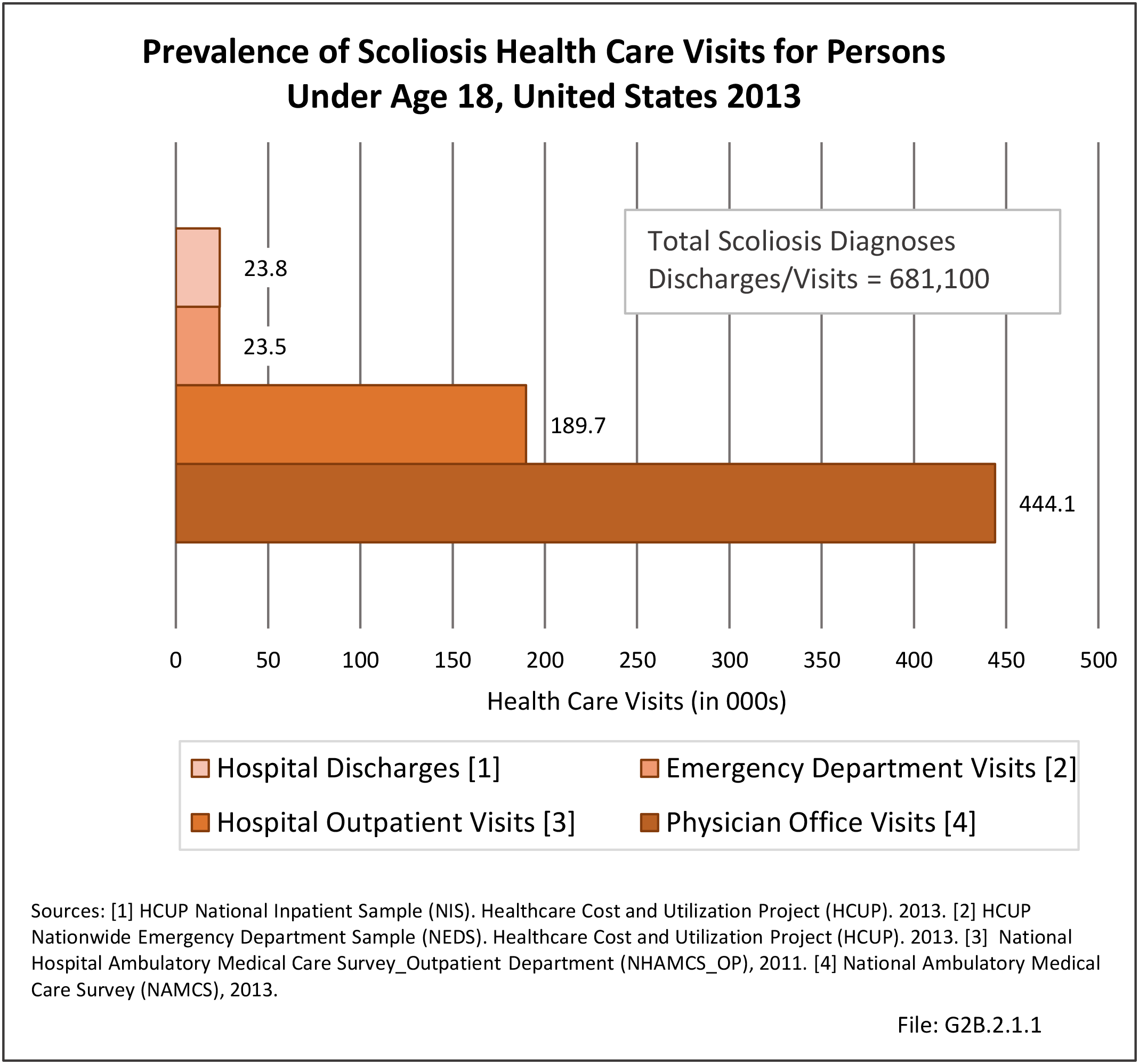
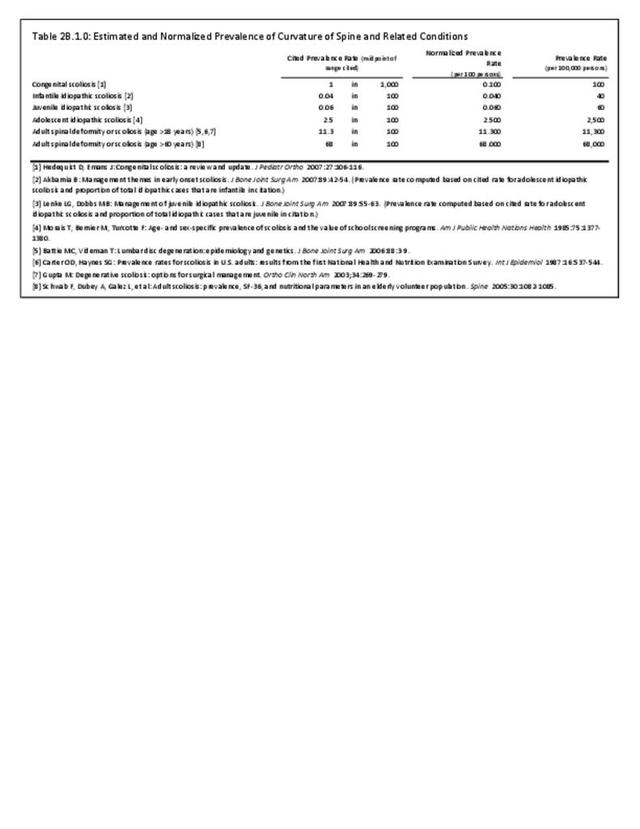
Spinal deformity and scoliosis can be found at birth due to genetic causes, develop during childhood, or occur late in life because of degenerative disc and joint disease. Common signs of scoliosis are a prominent shoulder or shoulder blade, or chest wall asymmetry. Another sign is uneven hips, with one hip seemingly higher than the other hip. It is important not to confuse scoliosis with poor posture and to realize that scoliosis will usually not disappear with age. Despite the severity of these conditions and the impact they have on the lives of children, the prevalence of spinal deformities in children under the age of 18 years is difficult to determine because of relatively low numbers and the degree to which the condition manifests initially in pain or disability. Estimated prevalence of spinal deformity conditions has been cited in numerous studies, and ranges from 0.4 in 1,000 for infantile idiopathic scoliosis1 to 2.5 in 1,000 for adolescent idiopathic scoliosis.2 (Reference Table 2B.1.0 PDF CSV)
There are several different types of scoliosis. The most common type of scoliosis is idiopathic, meaning the cause is unknown. Approximately 80% to 85% of scoliosis cases are idiopathic.3 Idiopathic scoliosis can occur as early as the first three years of life, which is known as infantile idiopathic scoliosis. If diagnosed between the ages of 4 to 10 years, it is known as juvenile idiopathic scoliosis, and from 10 years of age to skeletal maturity, as adolescent idiopathic scoliosis. The term “early onset scoliosis” (EOS) is also used to describe scoliosis that occurs prior to 10 years of age. Adolescent idiopathic scoliosis is the most common type.
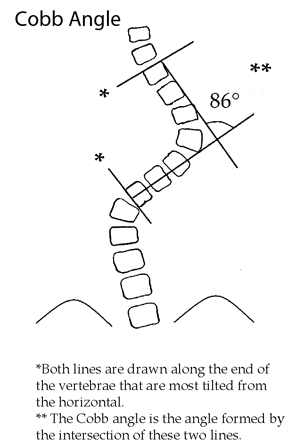
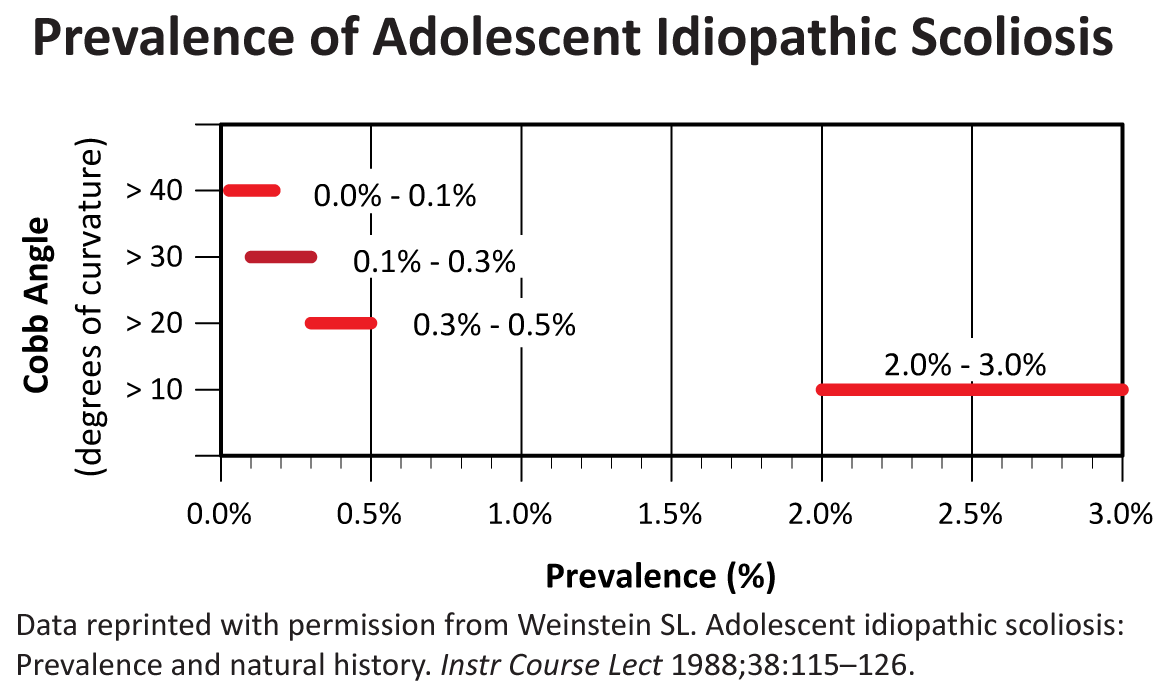
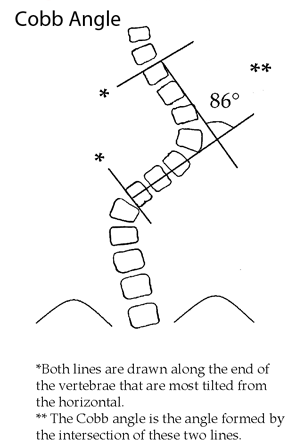
Scoliosis, if severe enough (>25°), is usually treated with bracing if the child is growing or with surgery if the curvature is more severe (>45° to 50°). The standard radiograph measurement method for all forms of scoliosis is the Cobb angle measurement technique, measured from the end plates of the maximally tilted end vertebral bodies in a standing radiograph.4 Whether the curve is >25° or >40° to 45°, the treatment is preventative in nature, helping to avoid progression of the curve and more significant future problems that might occur if it was left untreated. Increased mortality has been reported in untreated early onset scoliosis due to respiratory conditions.5 While this preventative aspect is hugely valuable and intuitively important, its benefit is difficult to measure from a public health standpoint, especially for rare conditions of childhood such as juvenile and adolescent pediatric scoliosis.
Infantile Idiopathic Scoliosis
Infantile scoliosis occurs in patients 0-3 years old and currently accounts for less than 1% of all cases of idiopathic scoliosis in the United States. Boys are affected by infantile idiopathic scoliosis at a higher rate than girls (3:2 ratio).1 Infantile scoliosis curves tend to be left-sided (75% to 90%). Past studies have indicated this rare type of scoliosis occurs more frequently in Europe than in North America.6
Treatment for patients with infantile idiopathic scoliosis is determined by anticipated or actual curve progression. Several common measurement techniques are used, with angles ≤20° generally considered at low risk for progression. In addition to measuring the Cobb angle, the rib-vertebra angle difference (RVAD) is used as a common predictor of curve progression.7 Patients with a Cobb angle of ≤25° and a RVAD of ≤20° are at a low risk for progression and should be re-evaluated every 4 to 6 months.1
Nonsurgical treatment, such as bracing or casting, is initiated if a curve progression of ≥10° occurs. Surgical treatment should be considered when nonsurgical measures, including both bracing and casting, are not successful. Surgical treatment is utilized when a curve is ≥45° and progressive in an immature child.1 Overall, surgical methods are continually evolving, with the goal of obtaining and maintaining curve correction while simultaneously preserving or encouraging spinal and trunk growth.
Surgical options currently utilized include various types of spinal fusion or hemiepiphysiodesis, a minimally invasive implant procedure to slow progression of curve growth. Additional techniques include growing-rod instrumentation (rods that expand and support the deformed spine) and vertical expandable (telescoping) prosthetic titanium rib (VEPTR) instrumentation.8 The goal of using surgical methods is to halt the progression of the curve and gain correction of the deformity, while allowing maximum growth of the spine, lungs, and thoracic cage.1 The allowance of normal lung development is one of the critical factors in recommending treatment for infantile and juvenile idiopathic scoliosis. Prevention of early mortality due to respiratory failure is a key driver of surgical treatment of early onset scoliosis.1,5
Juvenile Idiopathic Scoliosis
In 12% to 21% of idiopathic scoliosis cases, the diagnosis is made between 4 and 10 years of age. Between the ages of 4 and 6 years, the female-to-male ratio of juvenile idiopathic scoliosis is 1:1. However, the ratio of female to male cases rises to between 2:1 and 4:1 in children between the ages of 4 and 10 years, and to 8:1 in children who are 10 years of age or older.9 Both right and left curves are found with equal frequency for patients younger than 6 years, but rise to a 3:1 ratio of right versus left thoracic curves after the age of 6.10
Observation is the main treatment for patients with a small curve of less than 20° to 25°. Follow-up visits are recommended every 4, 6, 9, or 12 months, depending on the patient’s age, the degree of the curve, and the characteristics of the clinical deformity.9
Curves between 25° and 50° are usually treated with bracing in this age group. Bracing can be done either on a part- time or full-time basis, depending on the size of the curve as well as the age of the child. A study completed in 1982 evaluating the success of bracing reported an excellent prognosis when part-time bracing was utilized for patients with a curve of ≤35° and RVAD11 of ≤20°; however, curves ≥45° and RVAD of ≥20° had a less favorable prognosis for successful treatment with bracing.9
Overall, the curve patterns in patients with juvenile idiopathic scoliosis are similar to those with adolescent idiopathic scoliosis. Approximately 70% of patients with juvenile idiopathic scoliosis exhibit curve progression and require some form of treatment. In a study conducted in 1981, 55 of 98 patients (56%) with juvenile idiopathic scoliosis required spinal surgery. The most common and traditional surgery is posterior instrumentation and fusion.9
Adolescent Idiopathic Scoliosis
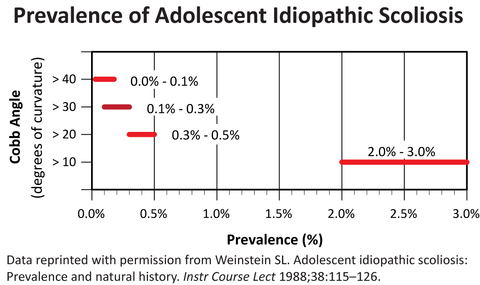
According to the Scoliosis Research Society (SRS), idiopathic scoliosis is diagnosed when a patient has asymmetry on forward bending combined with a curve of at least 10°.12 By this definition, the prevalence of adolescent idiopathic scoliosis in children from 11 to 18 years of age is 2% to 3%. Though the male-to-female ratio for smaller curves is about equal, larger curves seem to be more common in females. Similar results were found in a study conducted in 1985, where 29,195 children were screened for idiopathic scoliosis.2
Several studies have investigated the natural history and natural course of curve progression in adolescent idiopathic scoliosis. All report the strongest predictive factors in the development of idiopathic scoliosis are age, magnitude of curve, and gender.13,14,15,16 Girls are more likely to have adolescent idiopathic scoliosis than boys, and some studies report the onset is earlier in girls than boys. A factor highly correlated with curve progression is age at diagnosis; patients diagnosed at a younger age have a greater risk of curve progression. However, those diagnosed at a younger age seem to have a more favorable response to milder forms of treatment, which supports the practice of school screening to detect and lead to earlier diagnosis for those children who exhibit a smaller degree of curvature.
Treatment decisions for individuals with adolescent idiopathic scoliosis are made based on location, shape, pattern, and cause of the curve. The treatment choice is also a function of the patient’s future growth potential. Treatment choices include observation, bracing, and surgery. Observation is usually reserved for patients who have curves ≤25°. Bracing, which is used to stop curve progression (rather than for lasting correction of the curve), is usually used for patients who have curves ≥25° and who are still growing. Surgery is generally used for patients with curves ≥45°.
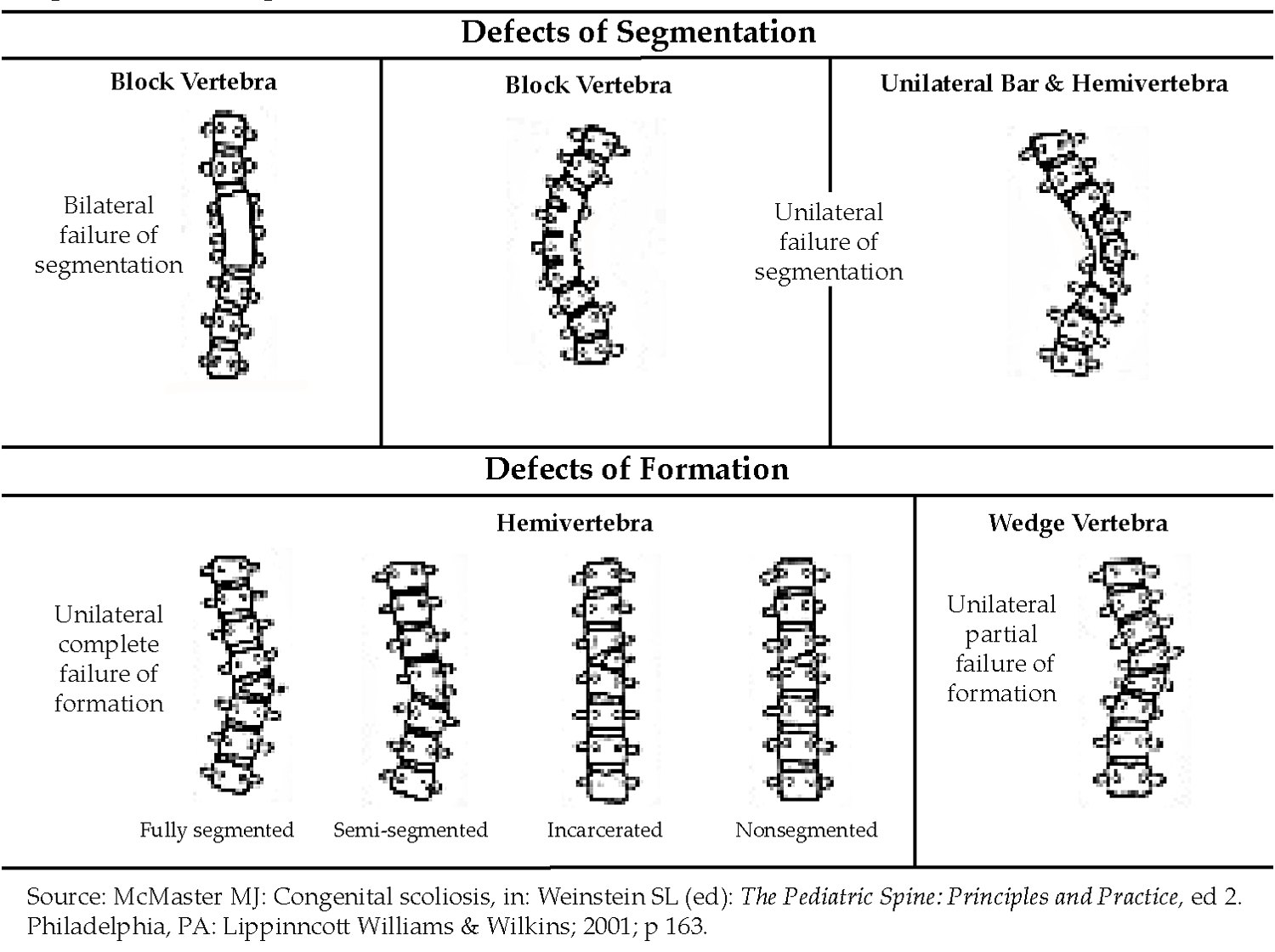
Congenital Scoliosis
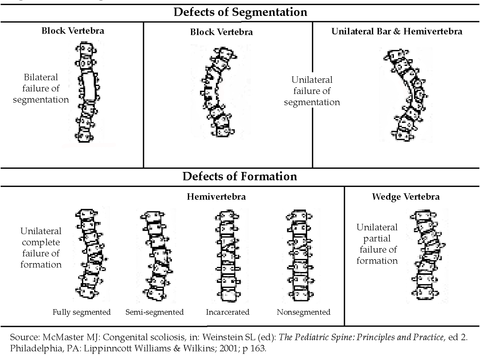
Congenital scoliosis is believed to affect approximately one child for every 1,000 live births.17 The cause is unknown in most cases, but in some cases, it is associated with various syndromes, as shown in the illustration below. Diagnosis occasionally is made during prenatal ultrasound. In cases of congenital scoliosis, additional congenital conditions, such as chest wall malformation or kidney or heart abnormalities, are often present. Treatment options for congenital scoliosis are bracing and/or surgery and are similar to treatments discussed for idiopathic scoliosis. Bracing is not as effective for congenital scoliosis as it is for idiopathic scoliosis.
Major abnormal spinal deformity occurring during infancy or early childhood poses a clinical problem because of the anticipated long growth period (at least 10 years), variable presentation and treatment methods, and the length of time that must pass before meaningful outcome results can be assessed in the small number of patients for definitive studies. Curves that result from congenital scoliosis are often not treated as easily as idiopathic curves because the deformity is in the bones rather than the soft tissue, causing the curve to be rigid.18
Neuromuscular
Scoliosis also occurs in conjunction with several congenital conditions that occur in infancy or childhood. These include muscular dystrophy, cerebral palsy, spina bifida, and spinal muscular atrophy. Scoliosis associated with these conditions is referred to as neuromuscular scoliosis. Both the likelihood and the severity of the scoliosis generally increases with the severity of the underlying condition. For example, a child with severe cerebral palsy who is unable to walk is more likely to have severe scoliosis than a child with mild cerebral palsy who can walk.
- 1. a. b. c. d. e. f. Akbarnia B. Management themes in early onset scoliosis. J Bone Joint Surg Am 2007;89:42-54. (Prevalence rate computed based on cited rate for adolescent idiopathic scoliosis and proportion of total idiopathic cases that are infantile in citation.)
- 2. a. b. Morais T, Bernier M, Turcotte F. Age- and sex-specific prevalence of scoliosis and the value of school screening programs. Am J Public Health Nations Health 1985;75:1377-1380.
- 3. Scoliosis Research Society (SRS). What is Scoliosis? https://www.srs.org/patients-and-families/conditions-and-treatments/pare... . Accessed October 3, 2019.
- 4. Herzenberg JE, Waanders NA, Closkey RF, et al. Cobb angle versus spinous process angle in adolescent idiopathic scoliosis: The relationship of the anterior and posterior deformities. Spine 1990;15:874-879.
- 5. a. b. Pehrsson, K., Larsson, S., Oden, A., & Nachemson, A. Long-term follow-up of patients with untreated scoliosis: A study of mortality, causes of death, and symptoms. Spine 1992;17(9):1091-1096.
- 6. Fernandes P, Weinstein SL. Natural history of early onset scoliosis. J Bone Joint Surg Am 2007;89:21-33.
- 7. Mehta M. The rib-vertebra angle in the early diagnosis between resolving and progressive infantile scoliosis. J Bone Joint Surg Br 1972;54:230-243.
- 8. Titanium Rib or VEPTR (Vertical Expandable Prosthetic Titanium Rib): An expandable titanium metal rod placed in a vertical position alongside the spine and attached to the ribs and pelvis or the spine. The VEPTR expands and supports a deformed chest wall cavity giving the lungs room to operate and grow. VEPTR is a new method for the treatment of thoracic insufficiency syndrome (TIS) and congenital spinal deformity (scoliosis) in children. Available at: http://www.ncbi.nlm.nih.gov/pubmed/15931035 . Accessed October 3, 2019.
- 9. a. b. c. d. Lenke LG, Dobbs MB. Management of juvenile idiopathic scoliosis. J Bone Joint Surg Am 2007;89:55-63.
- 10. Warner WC Jr. Juvenile idiopathic scoliosis, in Weinstein S, ed: The Pediatric Spine: Principles and Practice, ed 2. Philadelphia, PA: Lippincott Williams & Wilkins, 2001, p 330.
- 11. Rib vertical angle difference (RVAD): The rib vertical angle (RVA) is the angle formed by perpendicular line from apical vertebral end plate and a second line from the mid-neck to mid-head of the adjacent rib. The RVAD is the difference between the two RVA on the concave and convex sides of the curve. A curve greater than 20 is considered progressive. Available at: http://www.wheelessonline.com/ortho/congenital_scoliosis_and_vertebral_defects. Accessed October 3, 2019.
- 12. Lonstein J. Scoliosis: Surgical versus nonsurgical treatment. Clin Ortho Relat Res 2006;443:248-259.
- 13. Bunnell W. Spinal deformity. Pediatr Clin North Am 1986;33:1475-1487.
- 14. Weinstein S. Idiopathic scoliosis: Natural history. Spine 1986;11:780-783.[/fn[],fn]Karol LA, Johnston CE 2nd, Browne RH, Madison M. Progression of the curve in boys who have idiopathic scoliosis. J Bone Joint Surg Am 1993;75:1804-1810.
- 15. Porter SB, Blount BW. Pseudotumor of infancy and congenital mascular torticollis. Am Fam Physician 1995;52:1731-1736.
- 16. Willner S. Continuous screening and treatment of teenage scoliosis is recommended. Lakartidningen 1994;91:22.
- 17. Hedequist D, Emans J. Congenital scoliosis: A review and update. J Pediatr Orthop 2007;27:106-116.
- 18. Lonstein J. Scoliosis, in Lovell WW, Winter RB, Morrissy RT, Weinstein SL, eds: Lovell and Winter’s Pediatric Orthopaedics, ed 4. Philadelphia, PA: Lippincott Williams Wilkins, 1996, vol II.
Edition:
- Fourth Edition