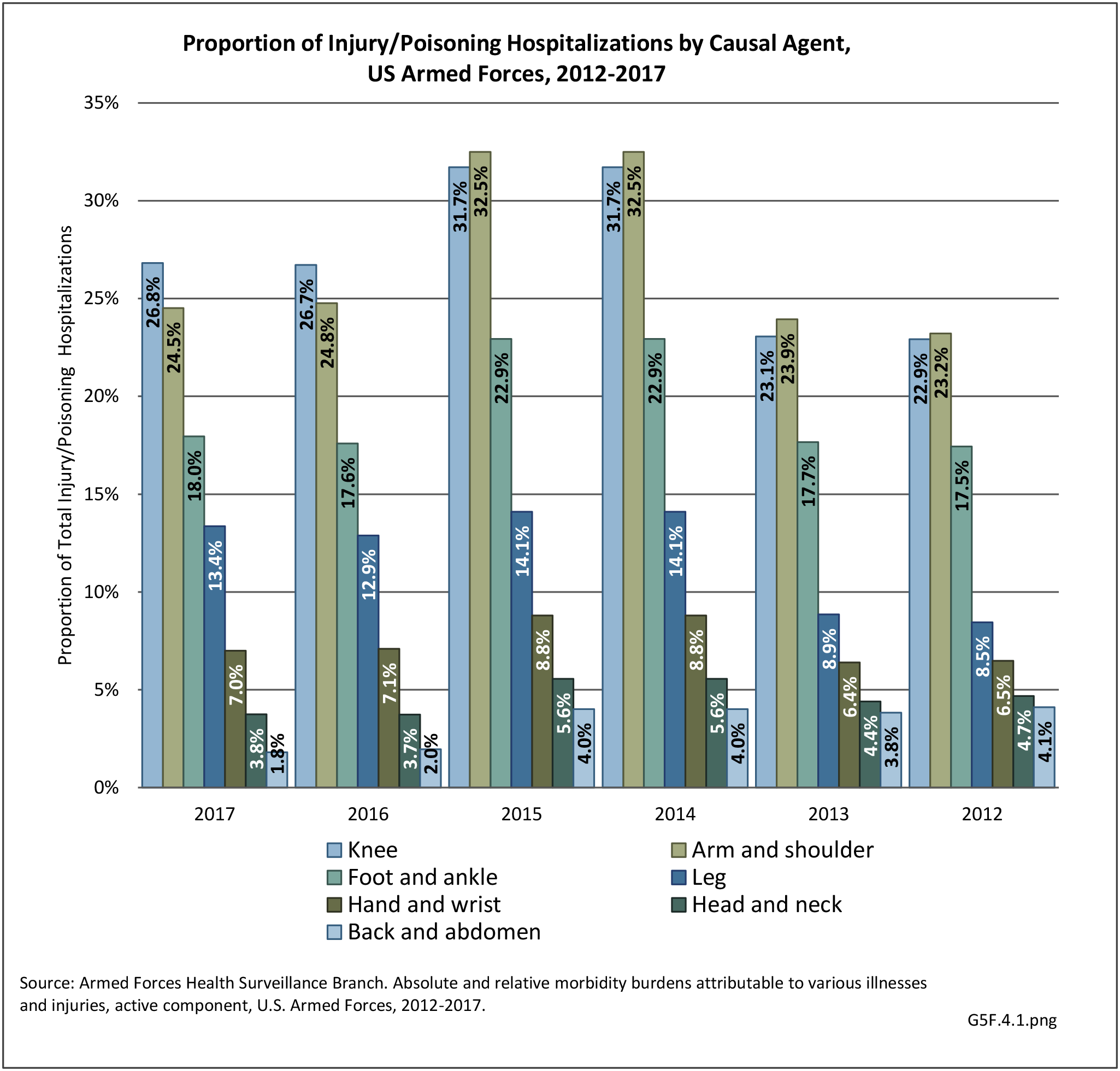
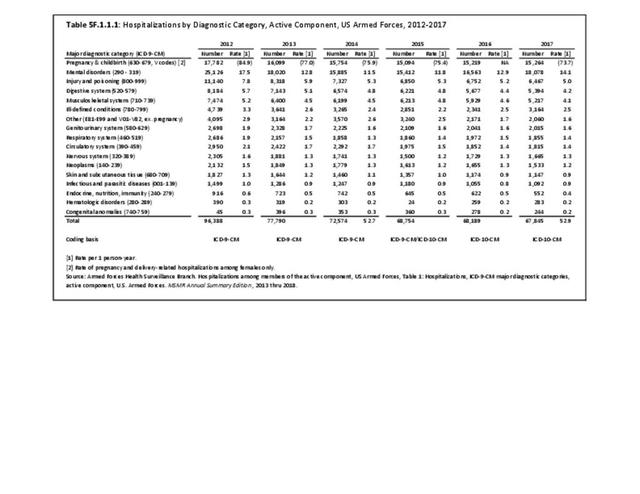
The military summary data presented here is largely derived from the Defense Medical Surveillance System (DMSS) from the Medical Surveillance Monthly Report (MSMR) annual reports on non-deployed, Active Duty United States military personnel. The DMSS examines total numbers of hospitalizations and ambulatory visits broken down by a defined set of diagnostic categories based on ICD-9-CM, and in the most recent years the ICD-10-CM, codes. In general, musculoskeletal injuries and conditions are compiled into two major diagnostic classifications, “injury and poisoning” or “musculoskeletal system” conditions. Typically, diagnoses included in the “injury and poisoning” category are more acute in nature (i.e. fractures, ligament tears, shoulder dislocations, etc.), while more chronic conditions (i.e. osteoarthritis, tendinitis, stress fractures, etc.) are included in the “musculoskeletal system” category.
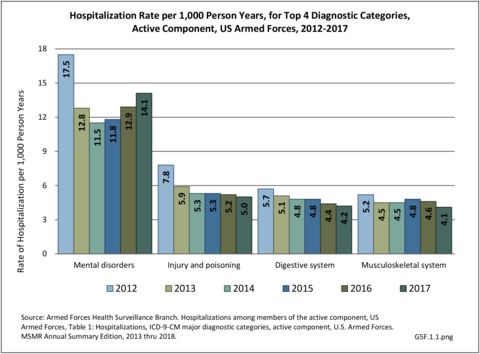
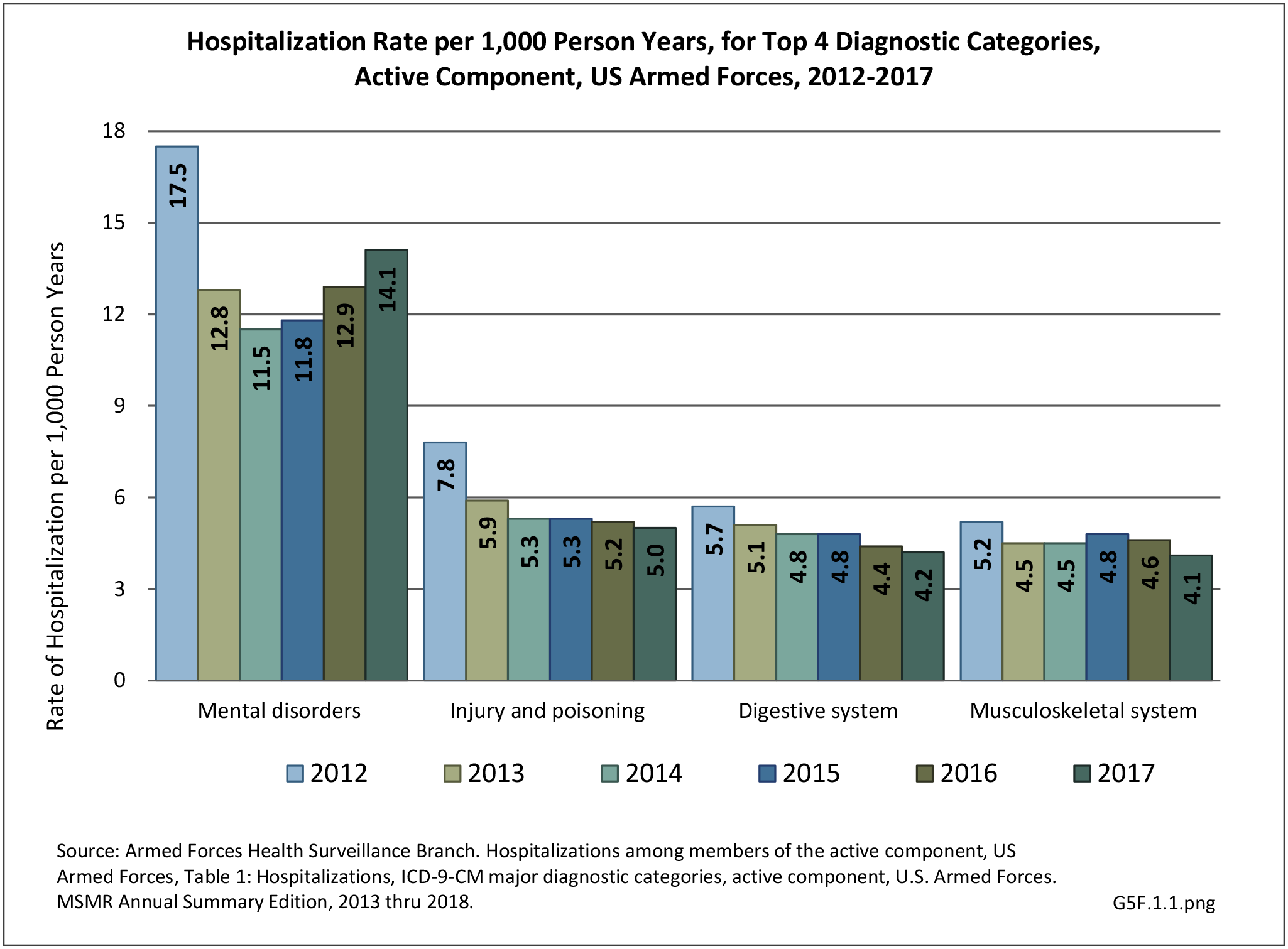
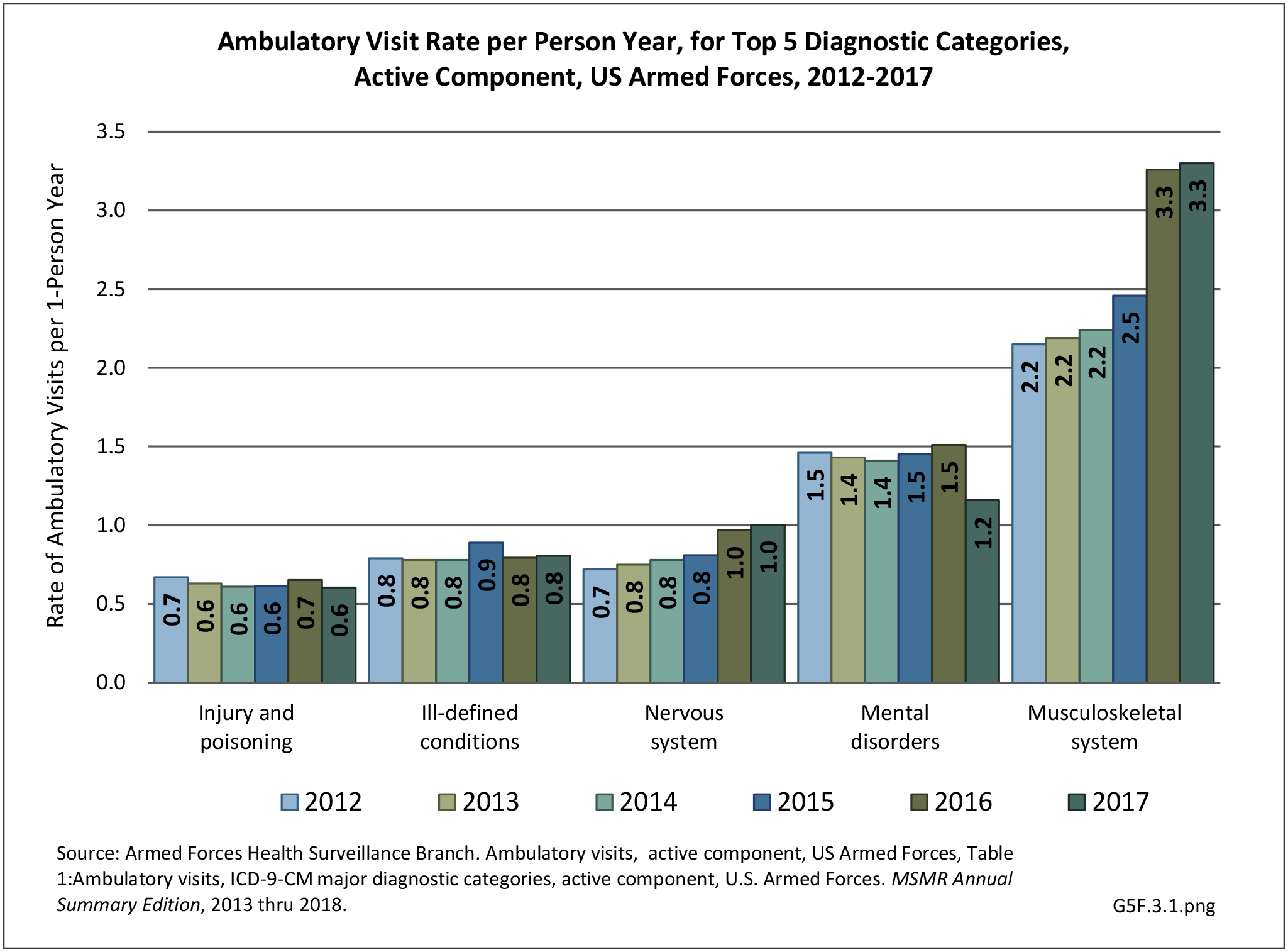
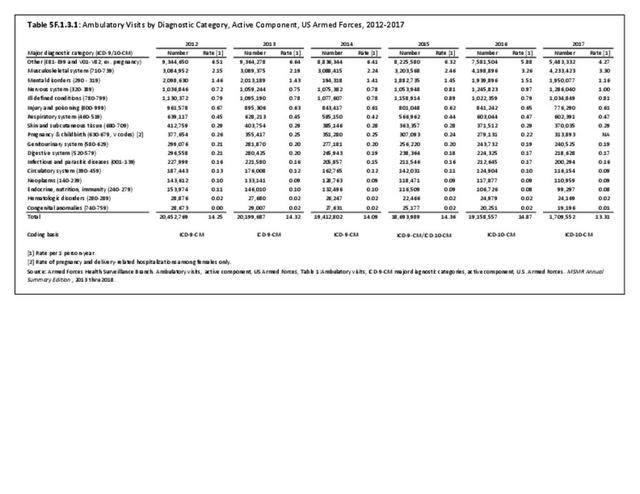
Excluding pregnancy-related visits, ”injury and poisoning” and “musculoskeletal system” are consistently amongst the top causes for hospitalization and consistently ranked second and fourth most frequent diagnoses across all military personnel. Mental disorders and digestive systems are commonly ranked first and third. This illustrates the significant overall burden of musculoskeletal problems in relation to all other medical conditions treated at Military Treatment Facilities (MTFs). (Reference Table 5F.1.1.1 PDF CSV)
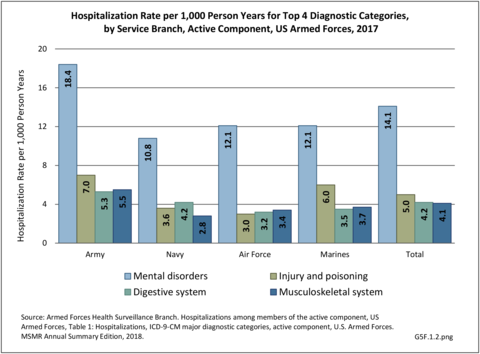
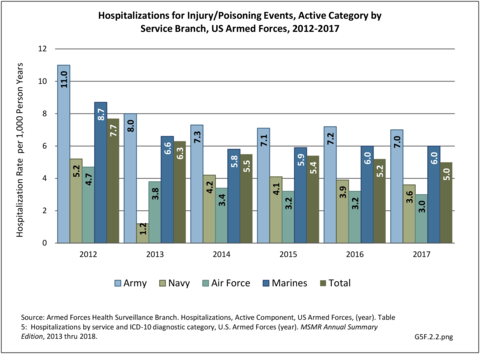
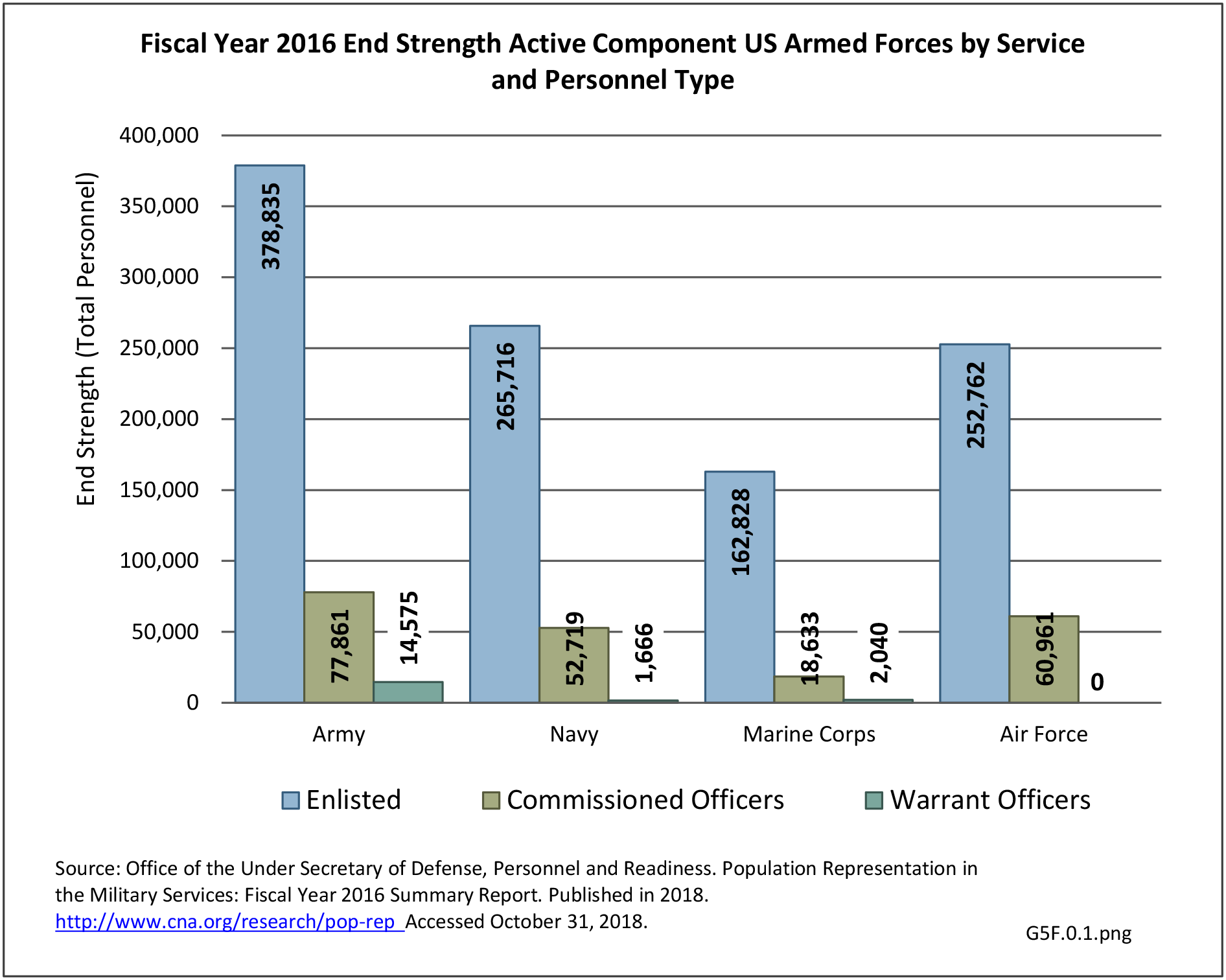
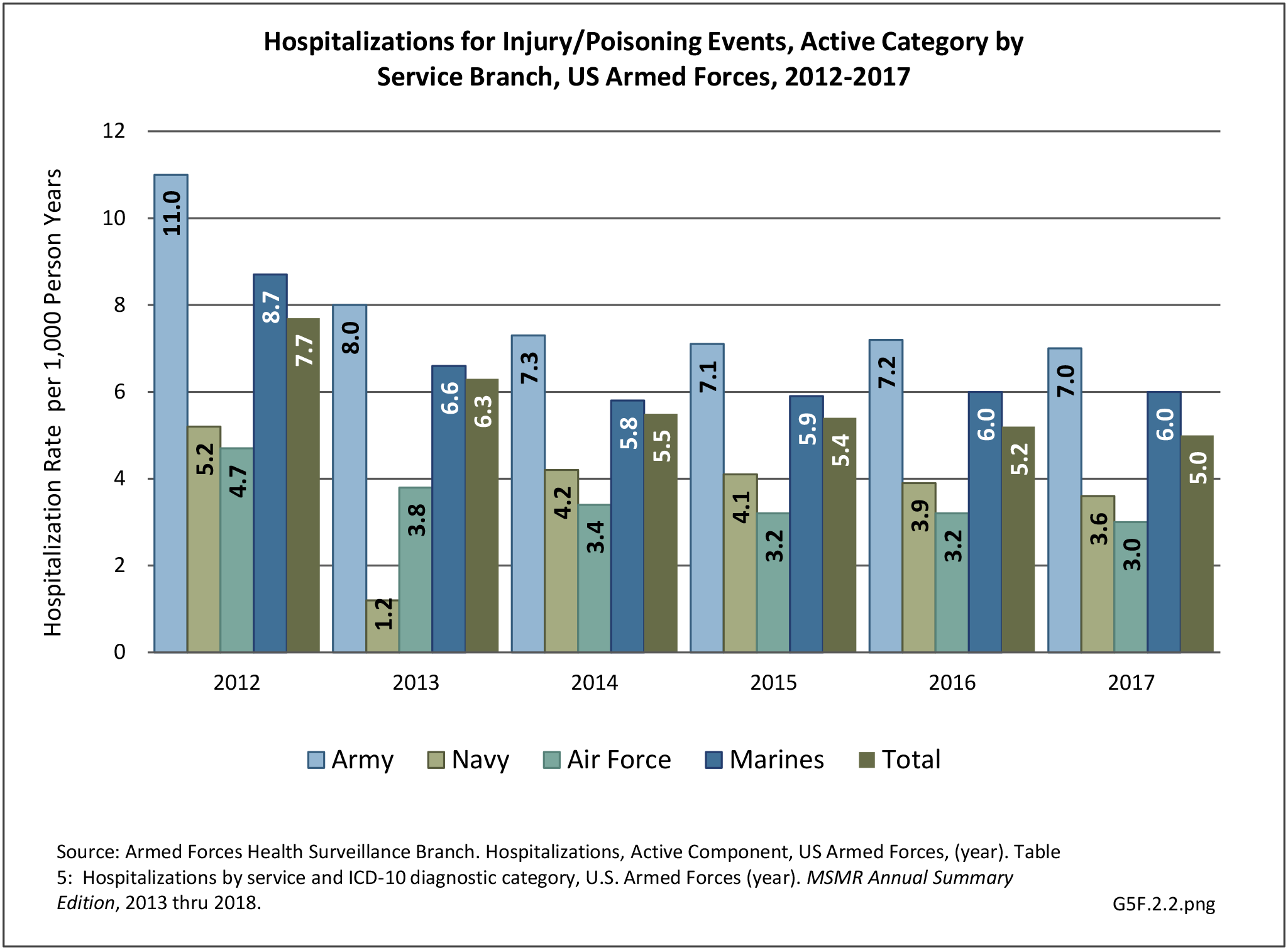
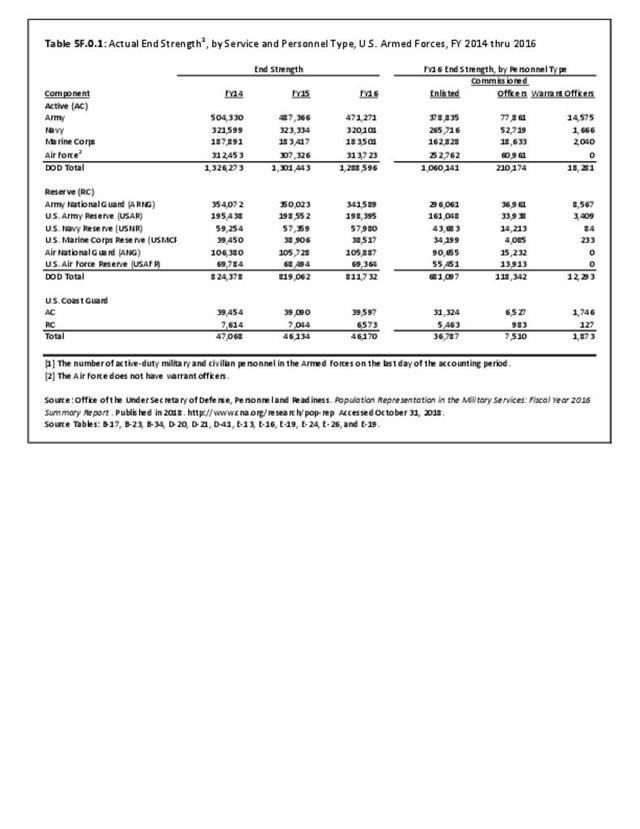
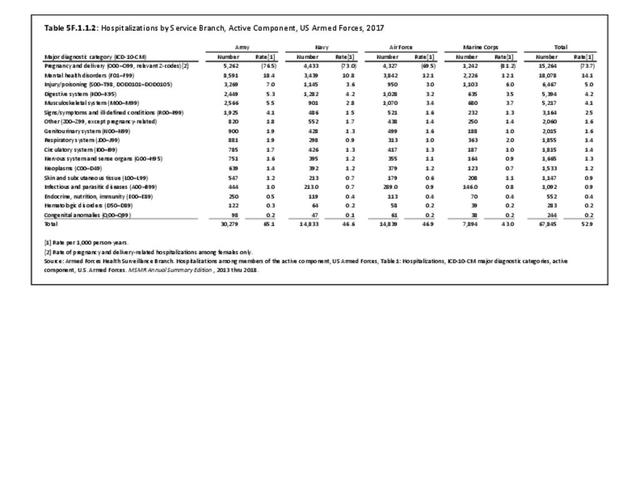
Broken down by service branch, the rate of hospitalization per person-year for all diagnostic categories is higher for Army personnel than for other service branches. Since the Army has more than double the number of personnel in other branches, the absolute number of hospitalizations is much higher and therefore not a valid comparison point. (Reference Table 5F.1.1.2 PDF CSV)
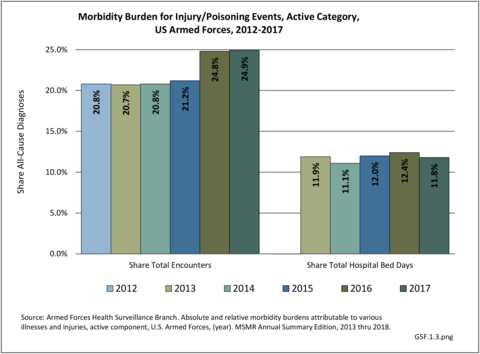
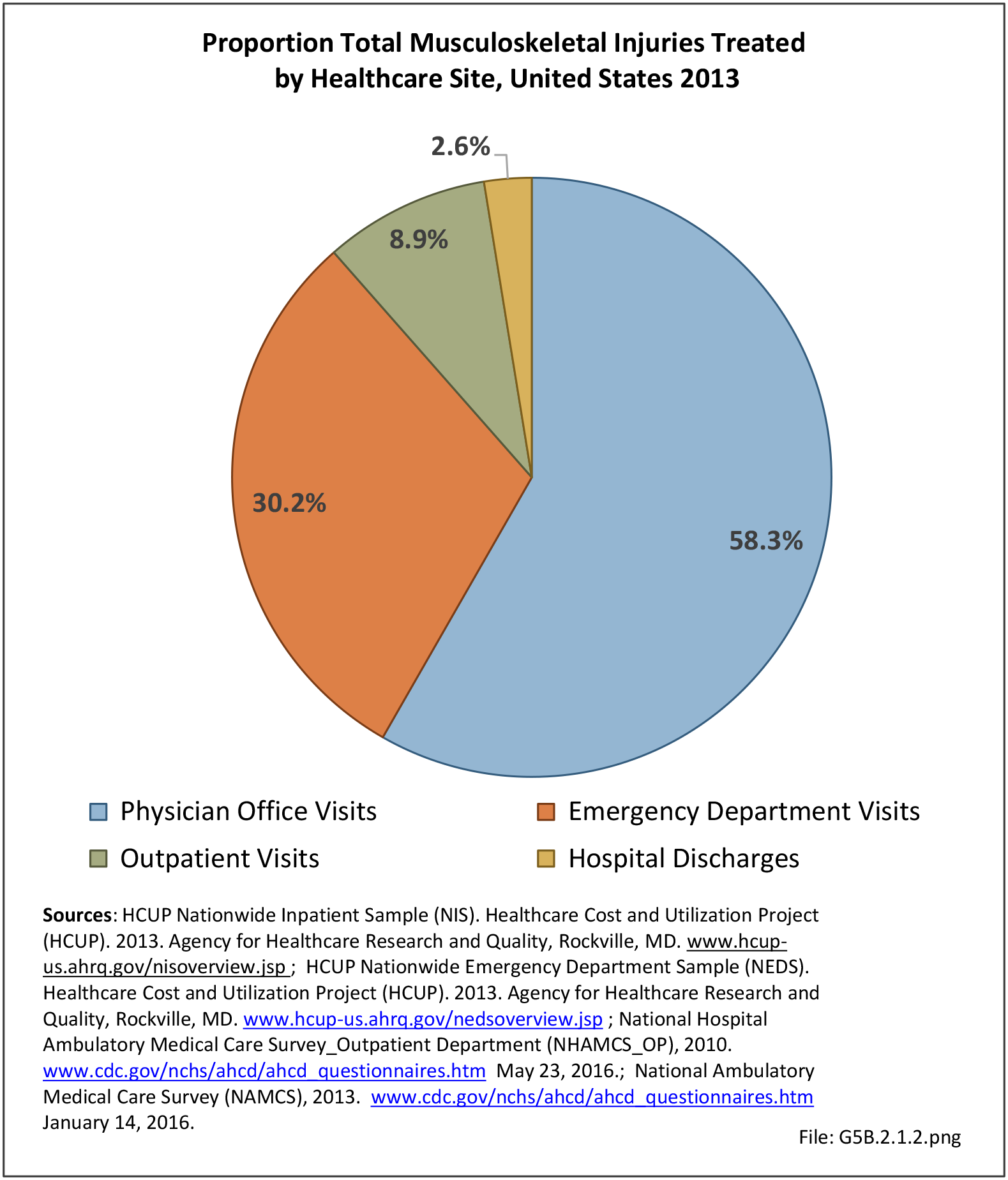
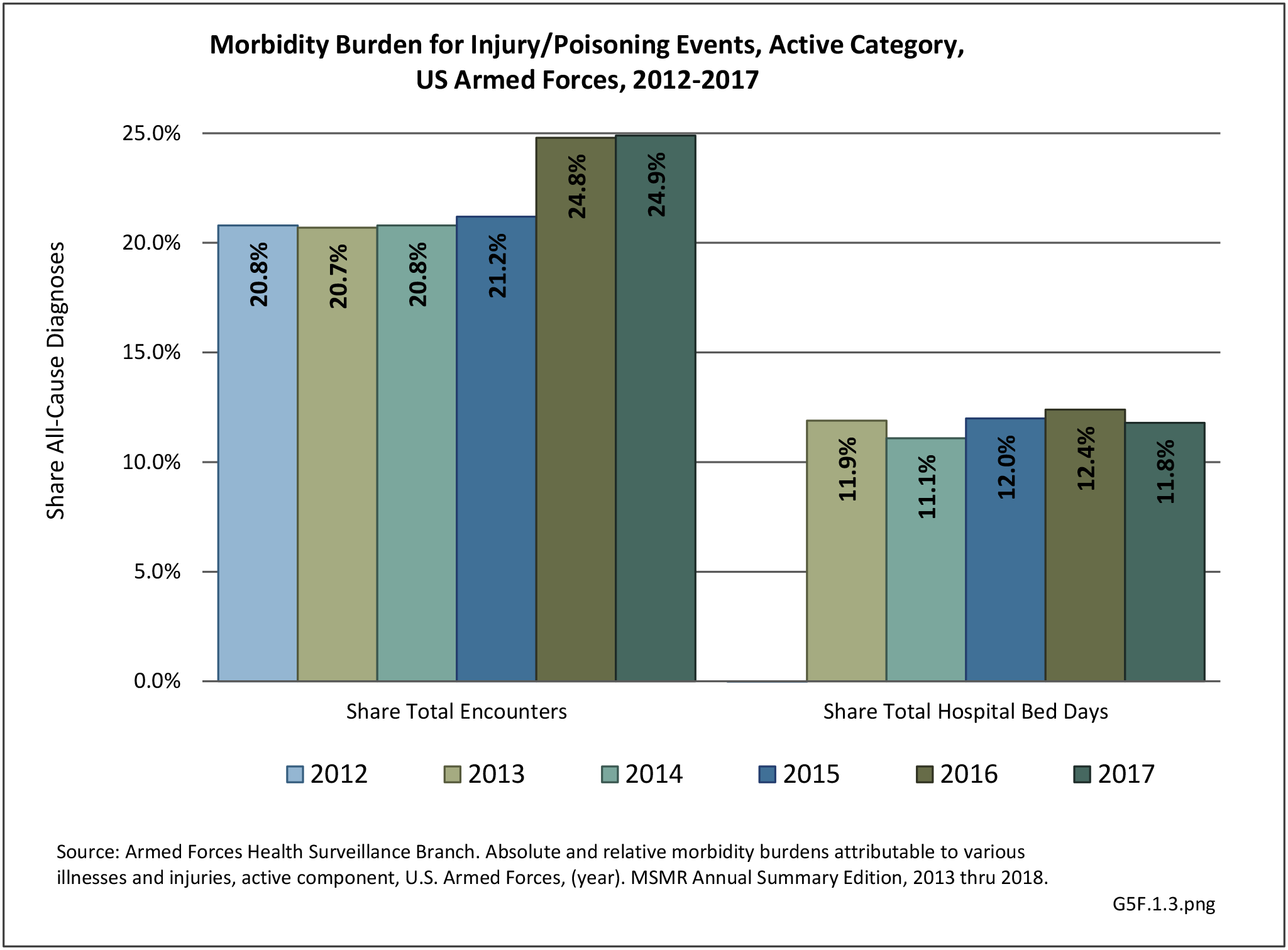
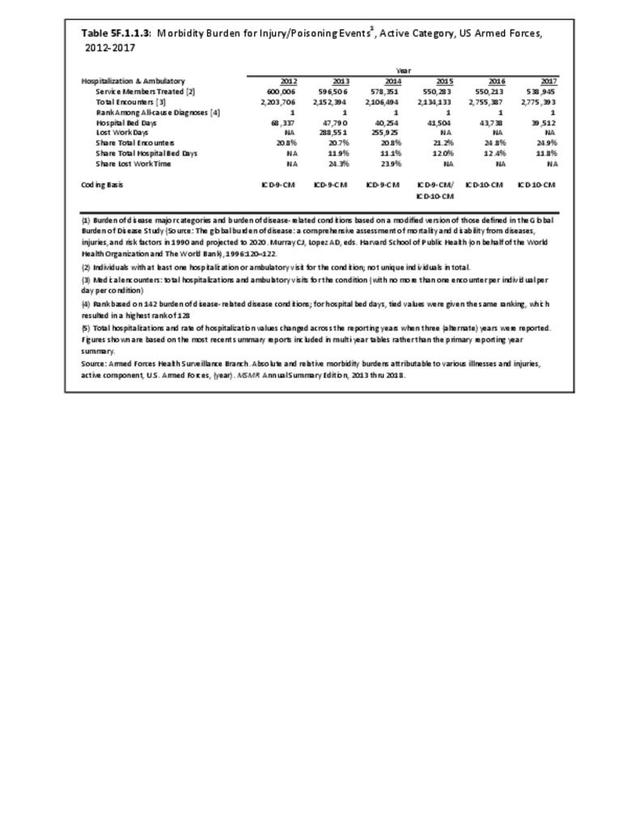
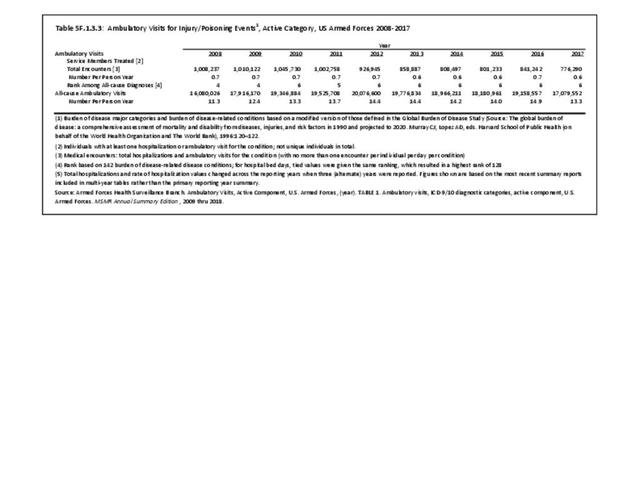
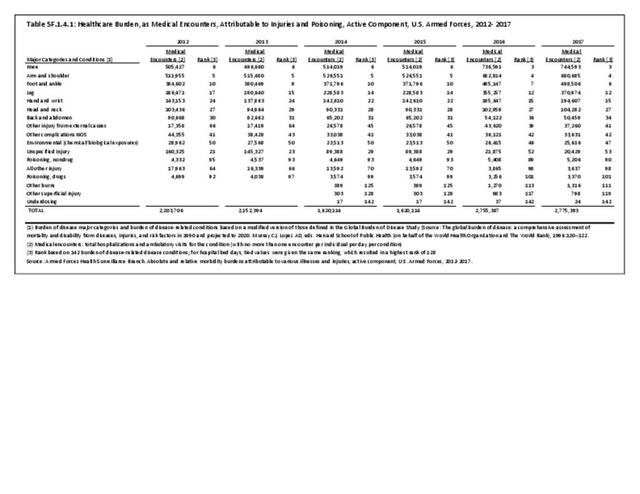
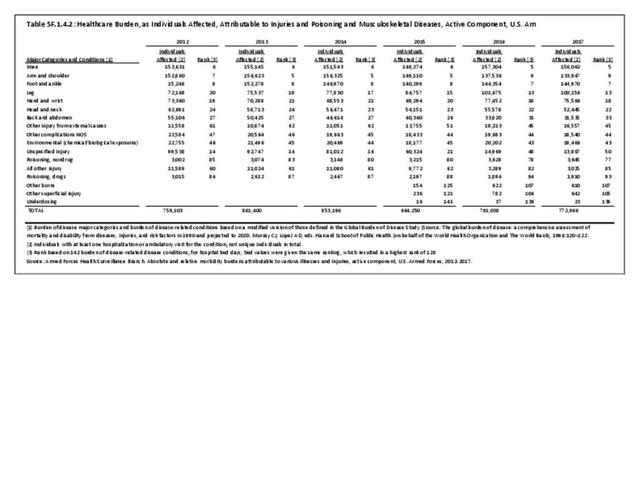
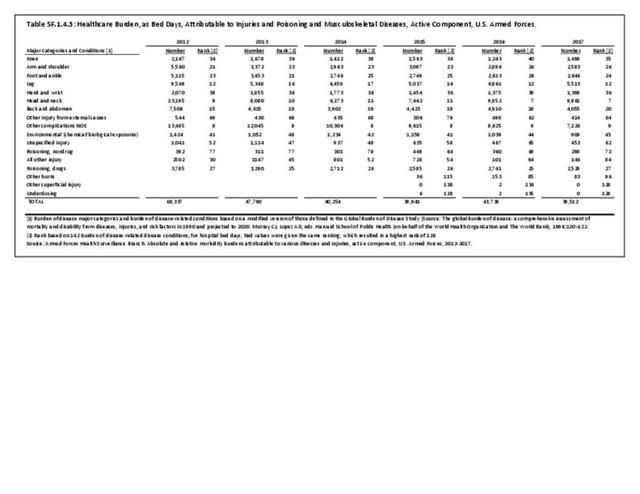
The total morbidity burden (hospitalizations plus ambulatory visits) for injury/poisoning events ranks as the number one cause of medical treatment received at MTFs. More than 540,000 service members were treated annually for an injury/poisoning event each year from 2012 to 2017. This accounted for roughly 25% of all encounters at military hospitals over that time frame. Additionally, injury/poisoning events resulted in 12% of hospital bed days and ultimately almost 25% of lost work time. (Reference Table 5F.1.1.3 PDF CSV)
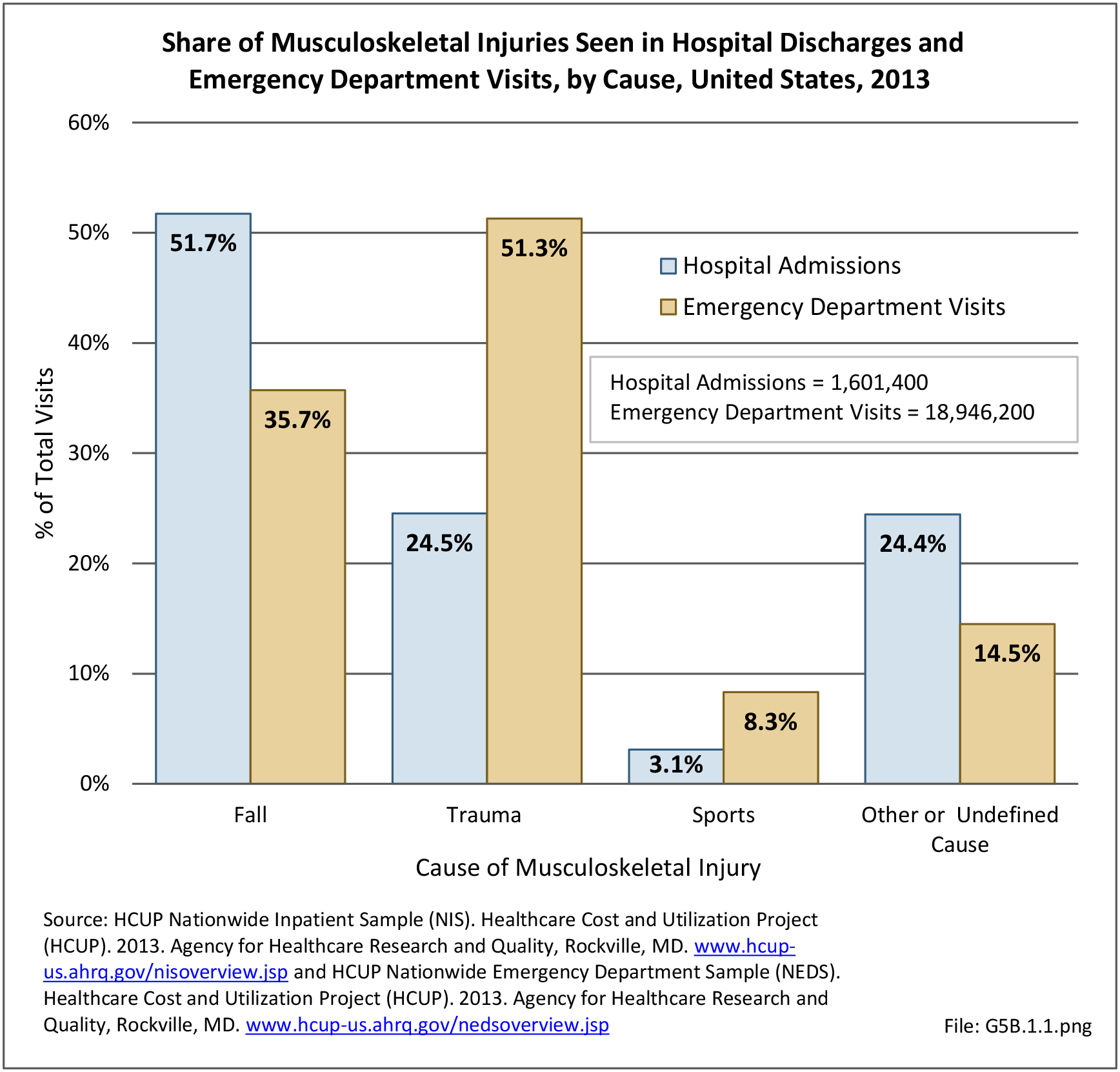
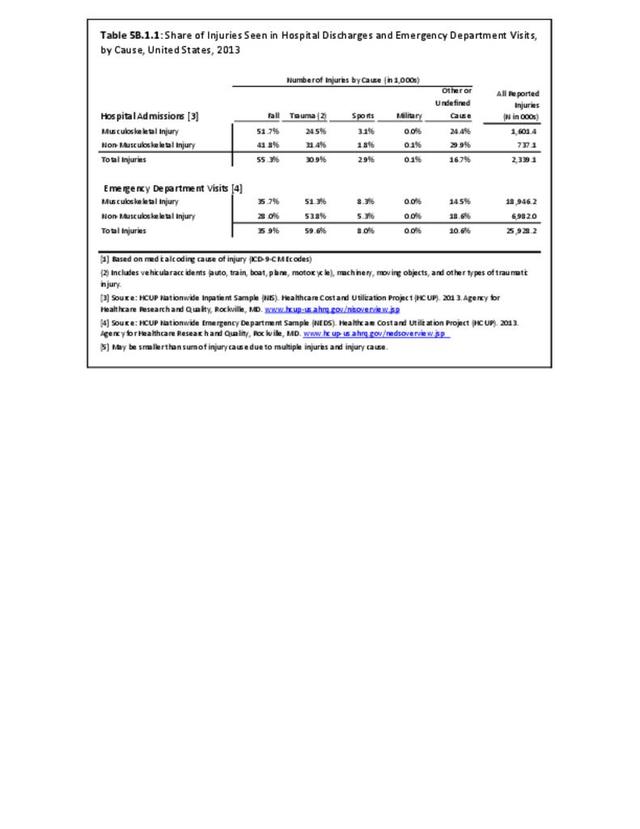
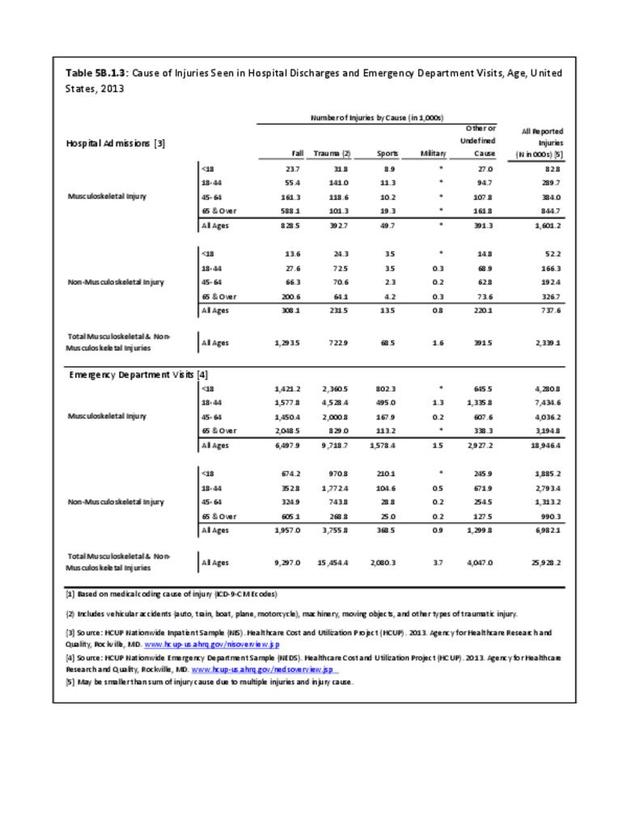
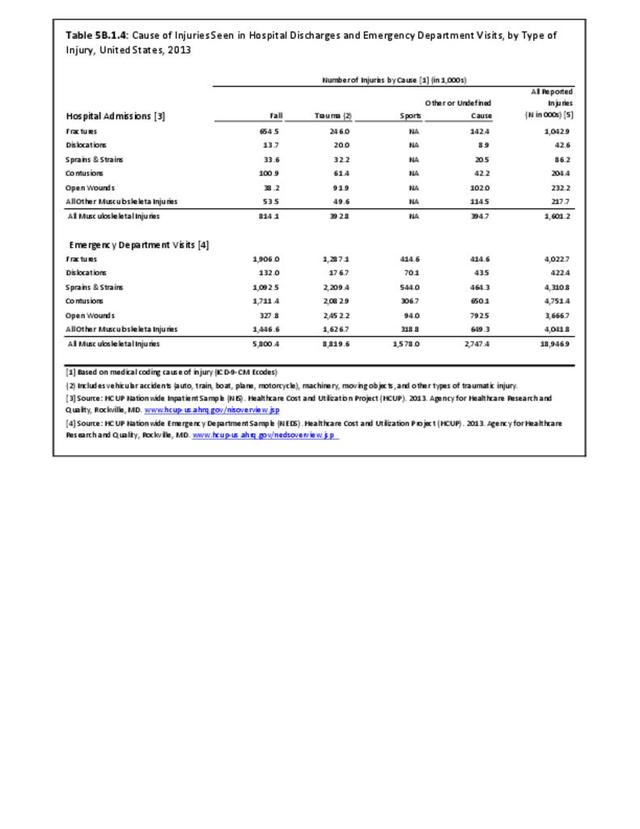
Cause of Hospital Visits
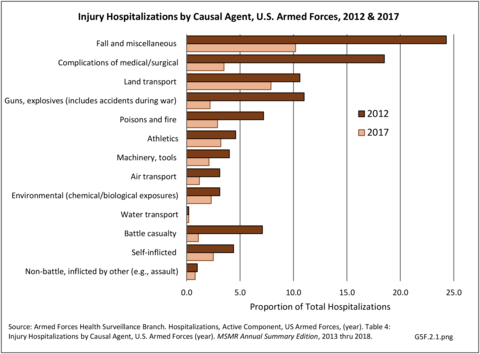
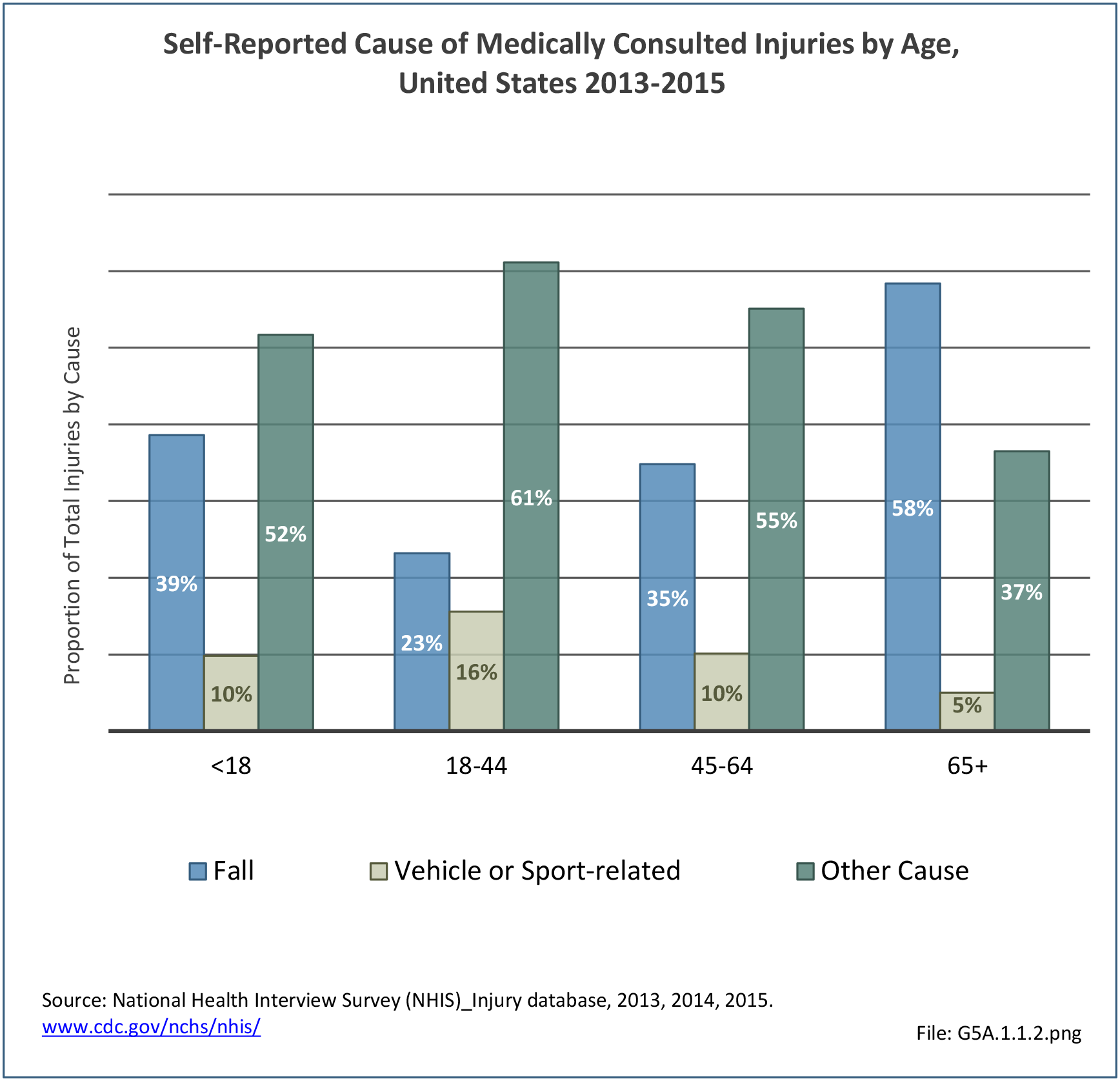
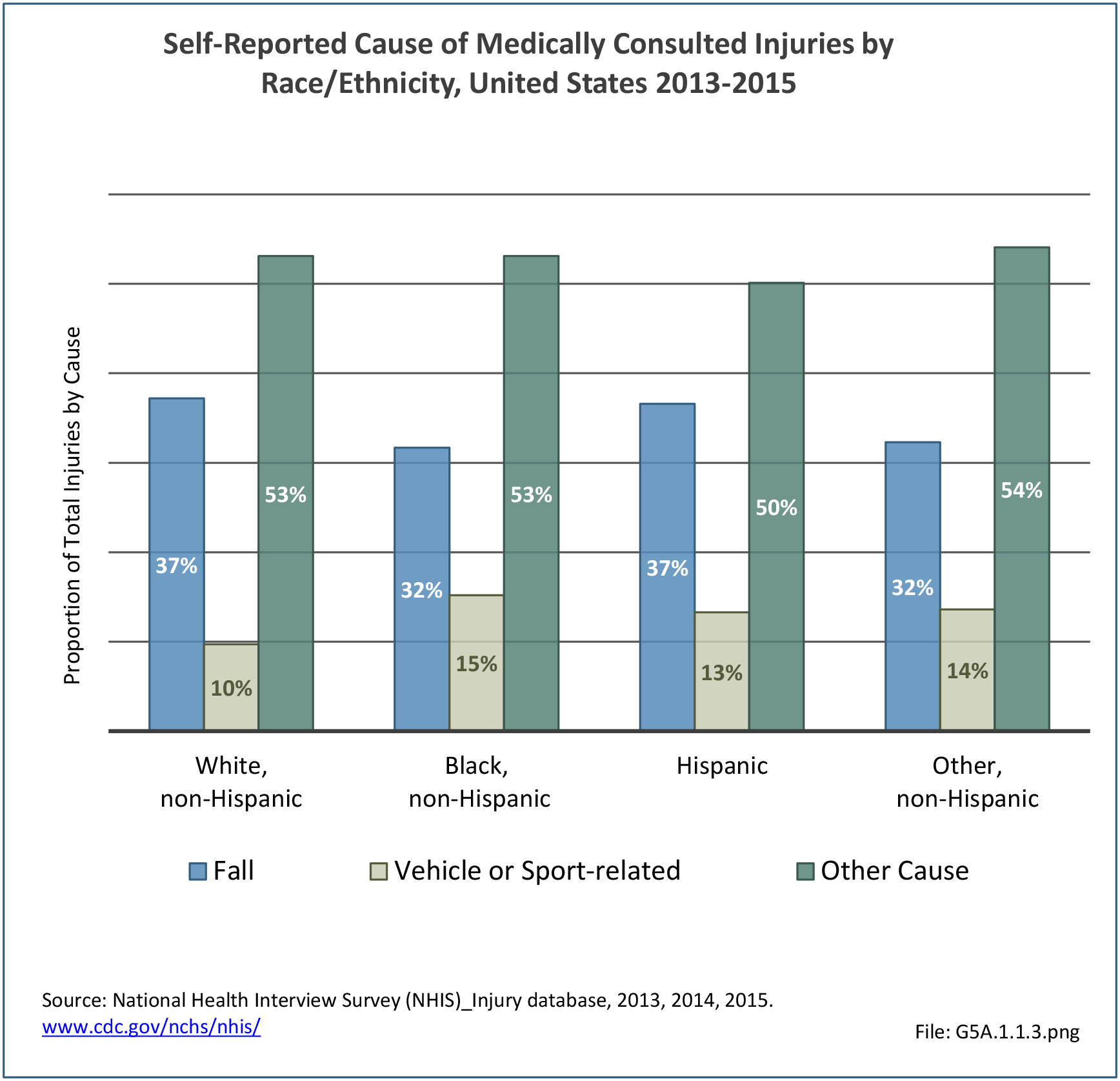
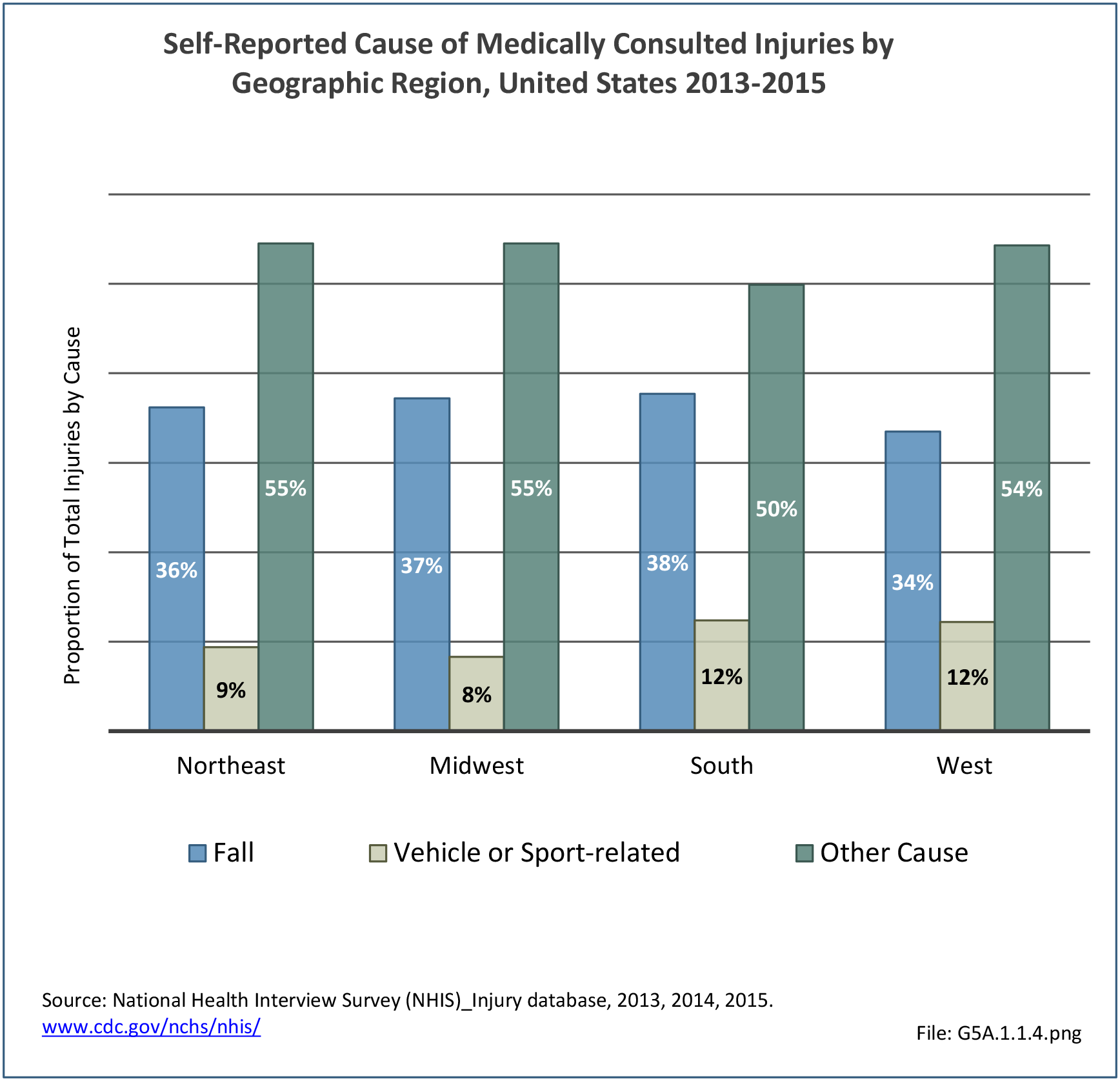
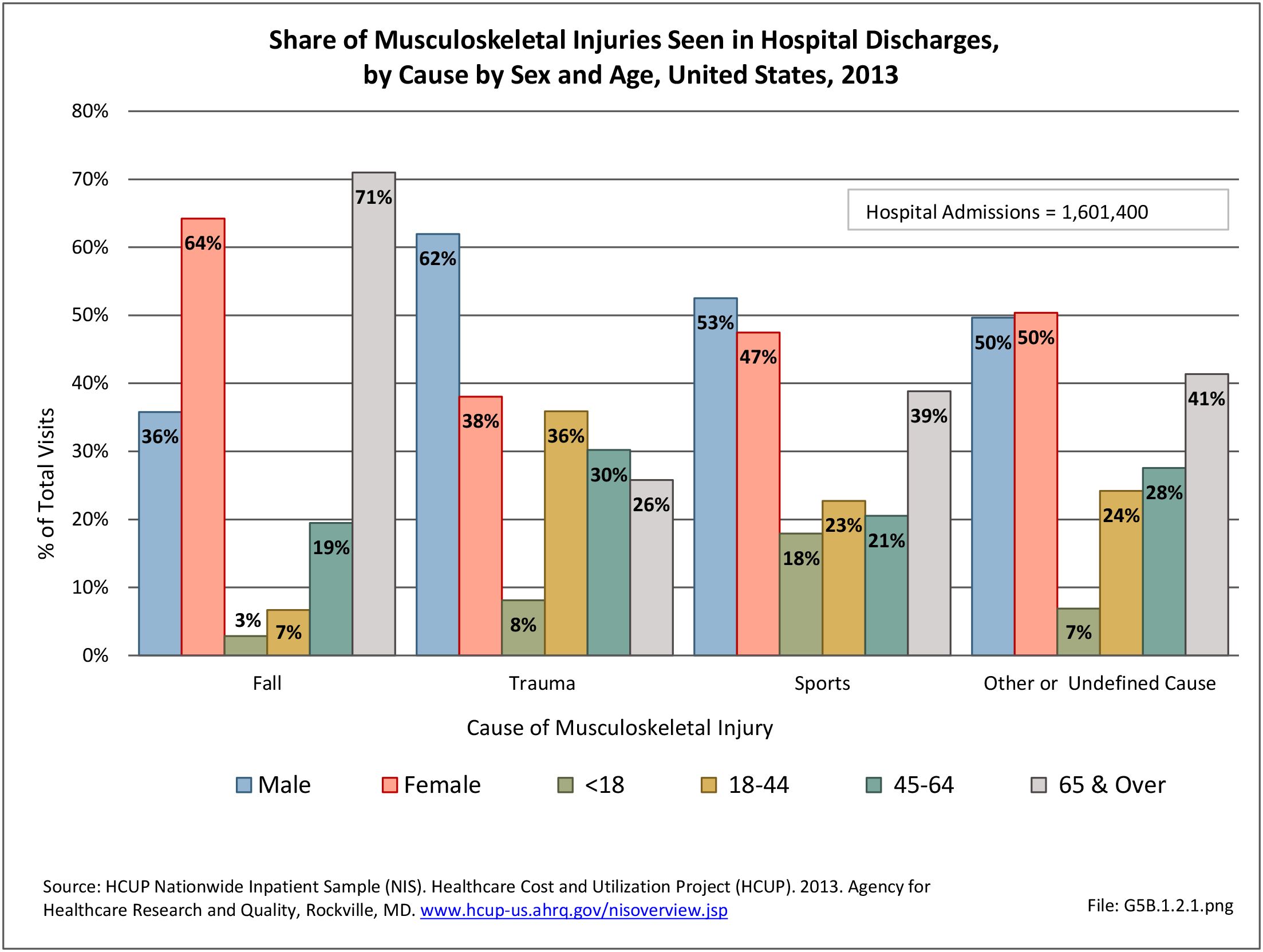
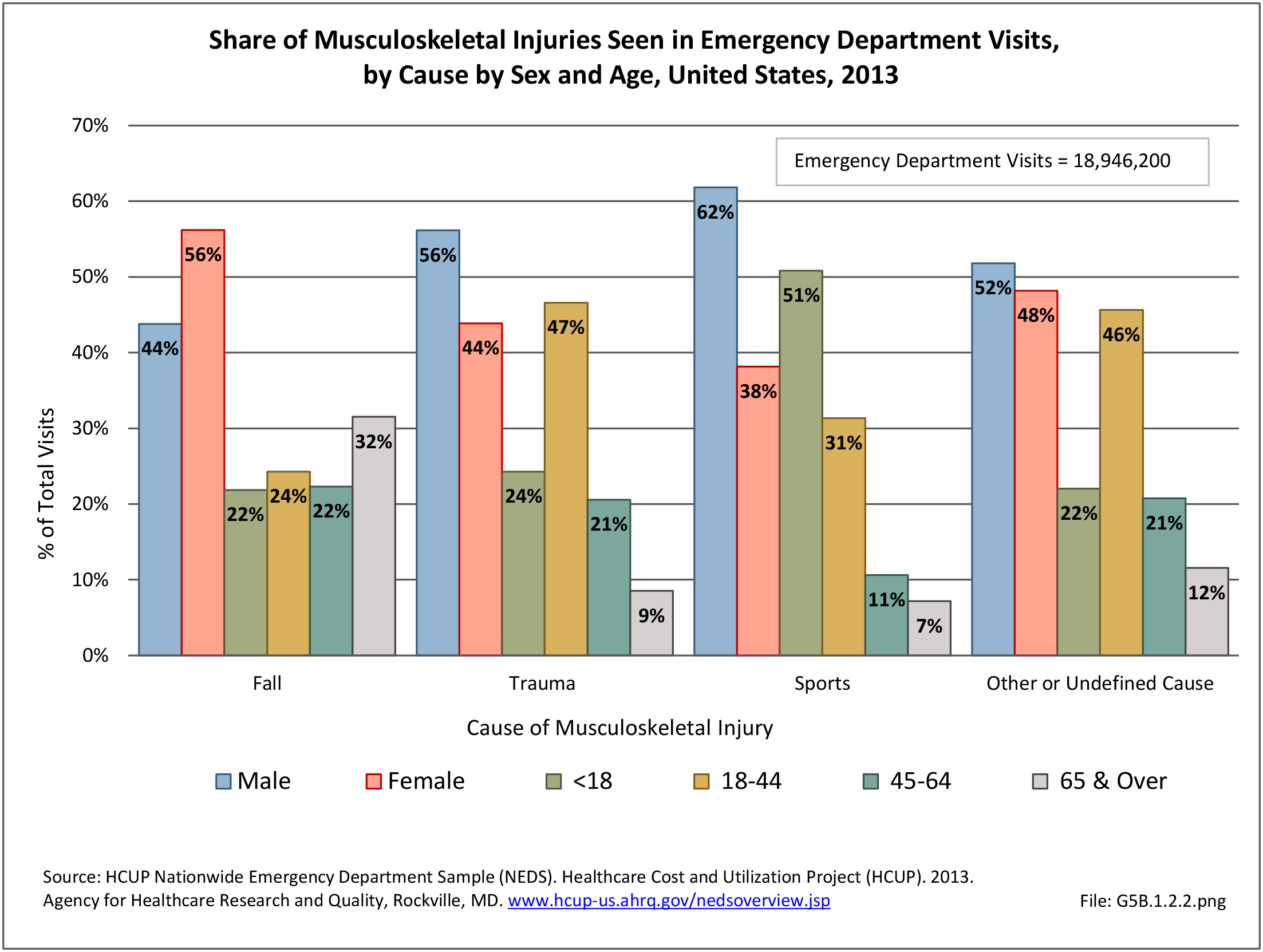
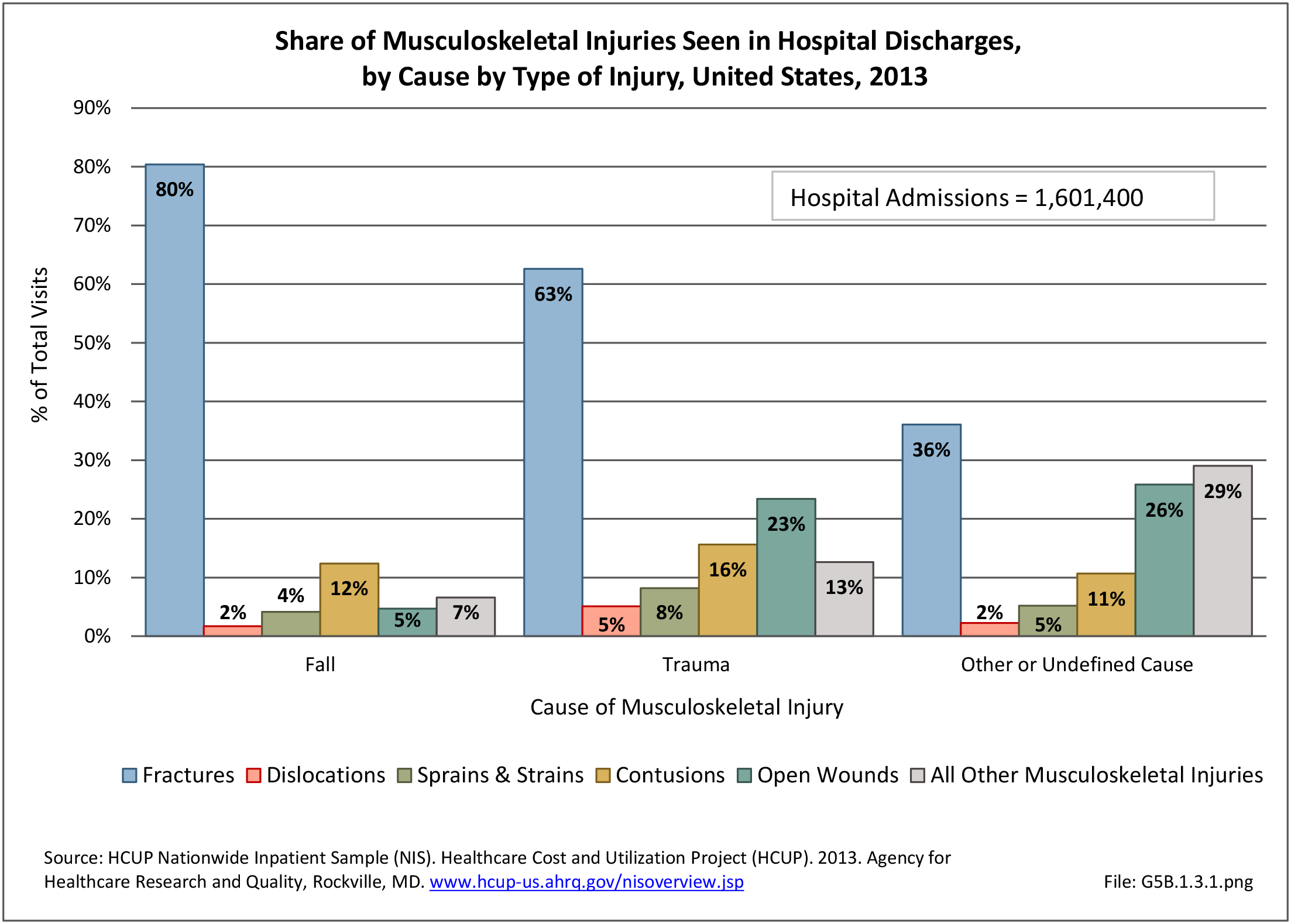
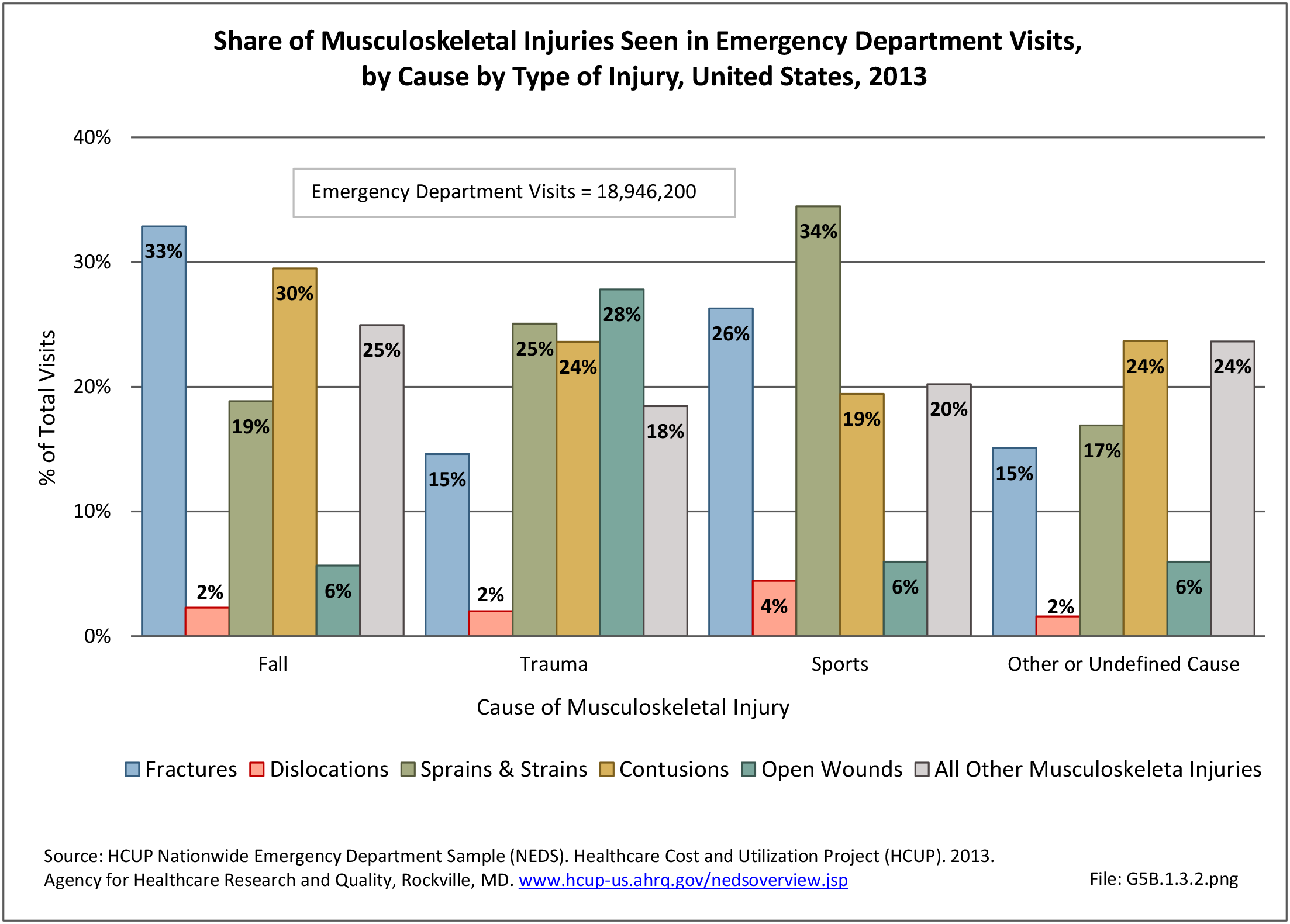
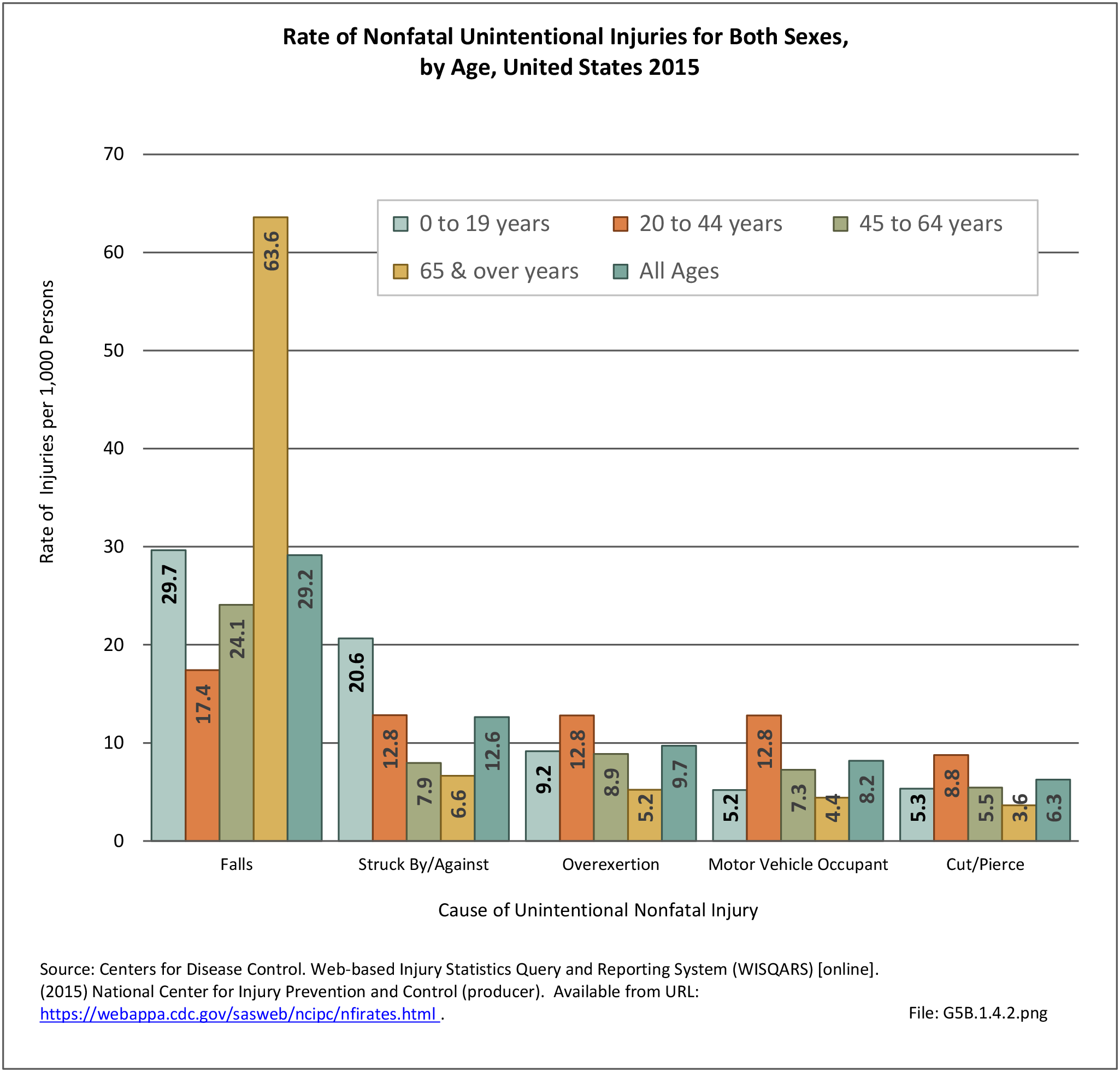
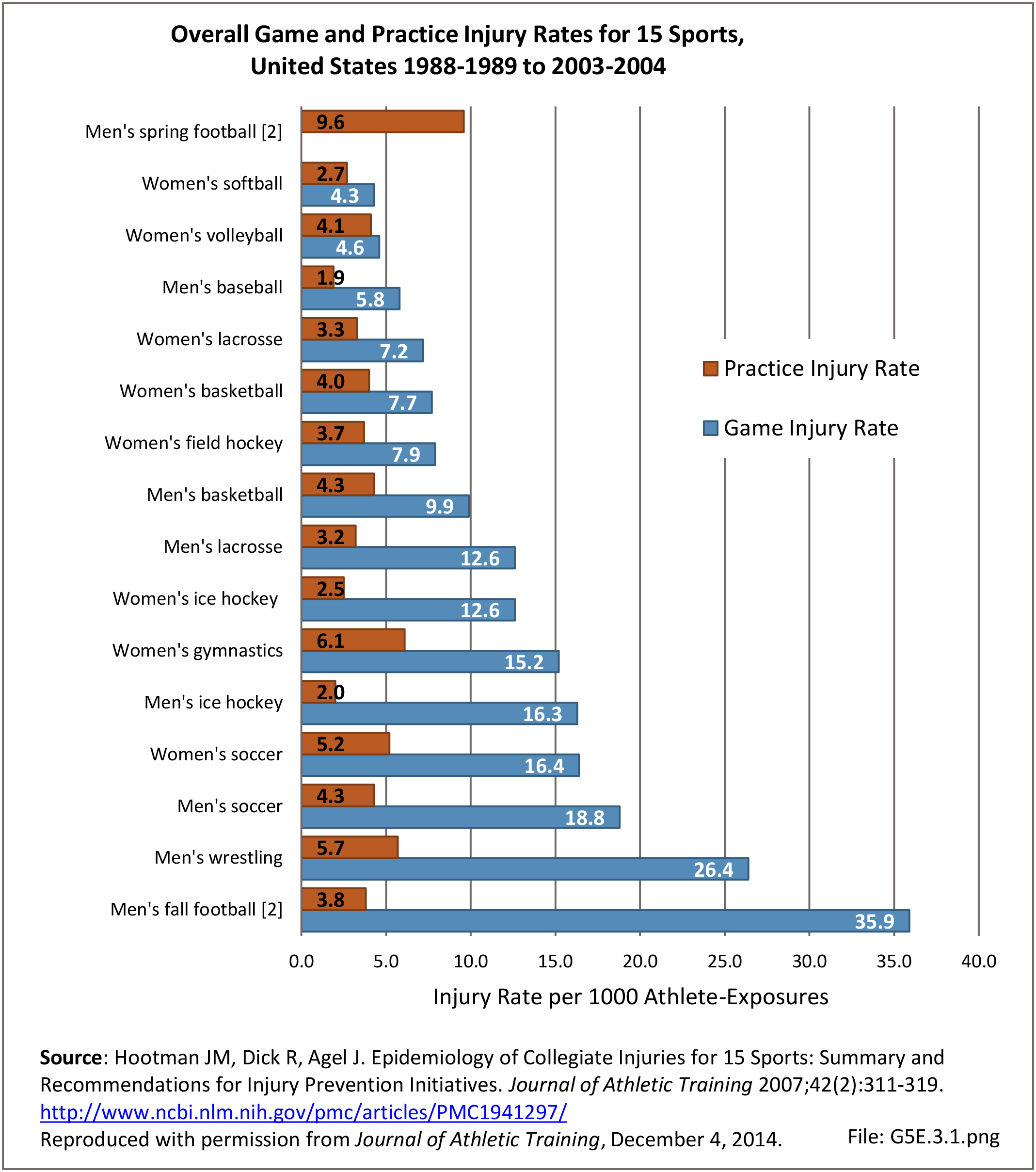
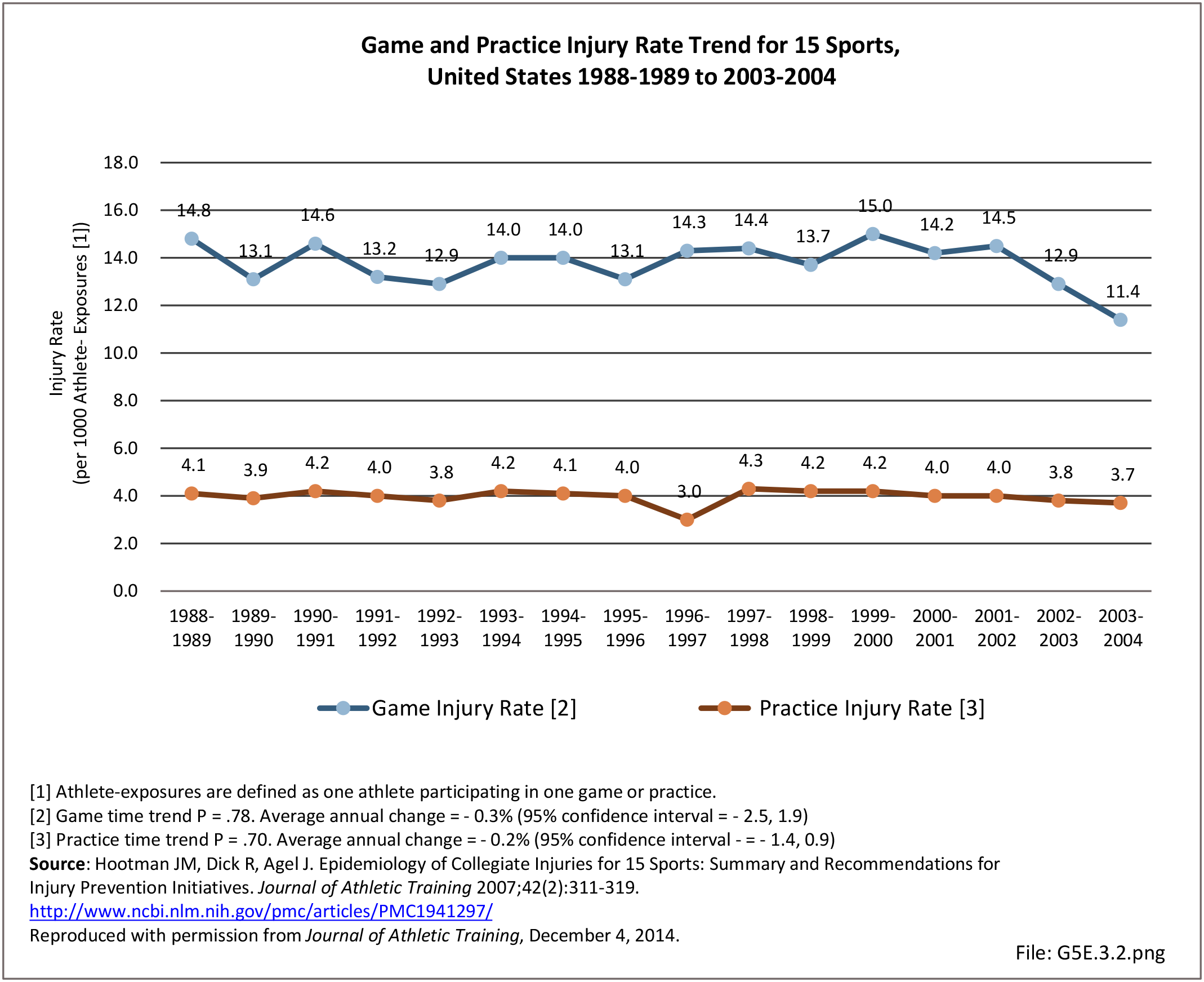
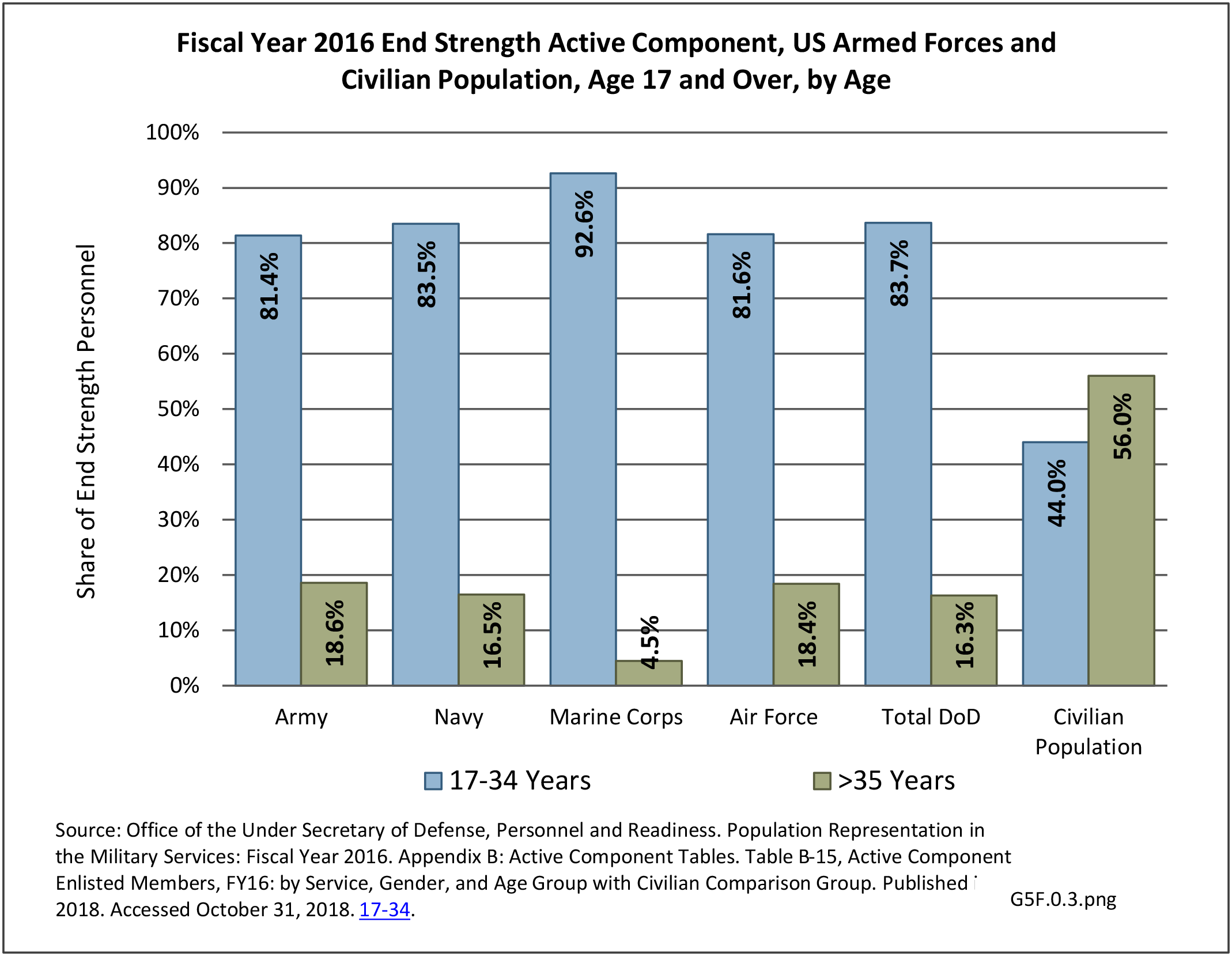
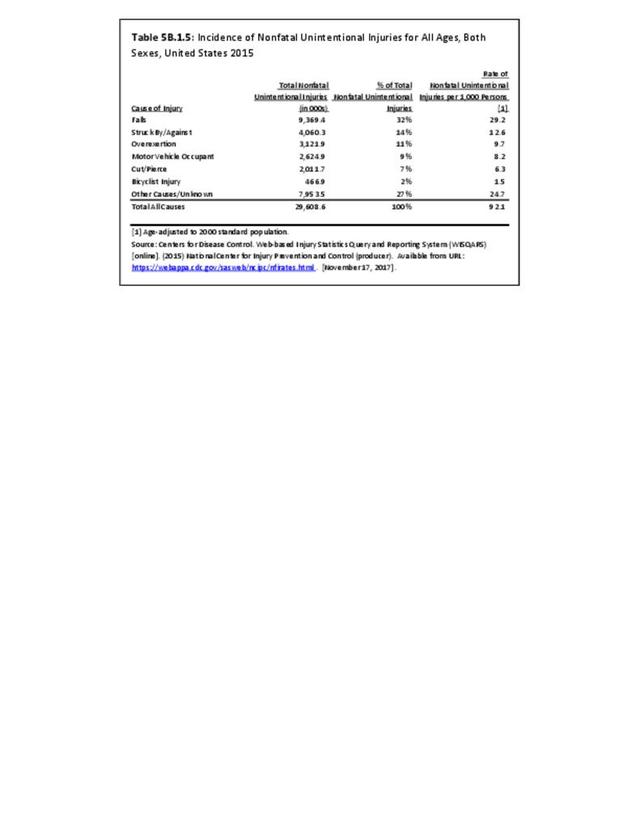
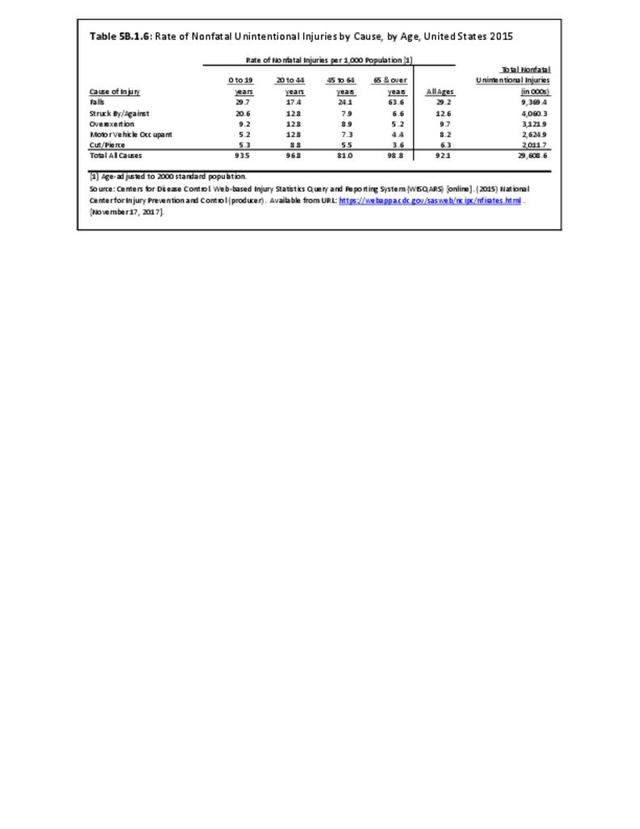
Musculoskeletal injuries in the military encompass a wide range of pathology from chronic overuse conditions to acute injuries from training accidents to high energy blast injuries sustained on deployments. Given the overall young age of military cohorts, injuries sustained are often sports or training related and not unlike what would be seen in a civilian Sports Medicine practice; however, these injuries often occur at a higher incidence when compared with their civilian counterparts. The high energy blast injuries that we grew accustomed to during the heights of the Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) conflicts have decreased over the last decade yet still remain a significant cause for morbidity and mortality amongst the military population.1
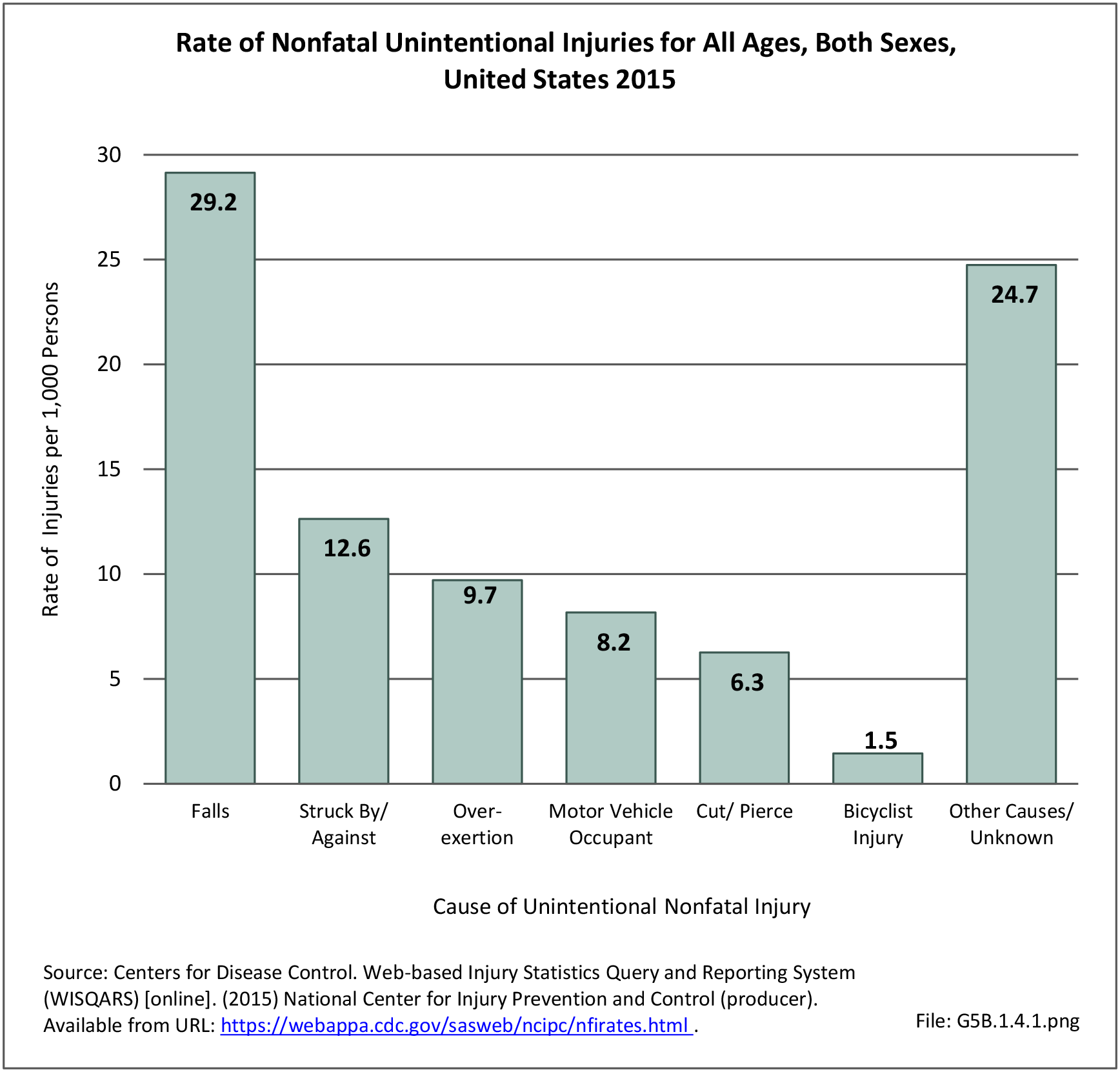
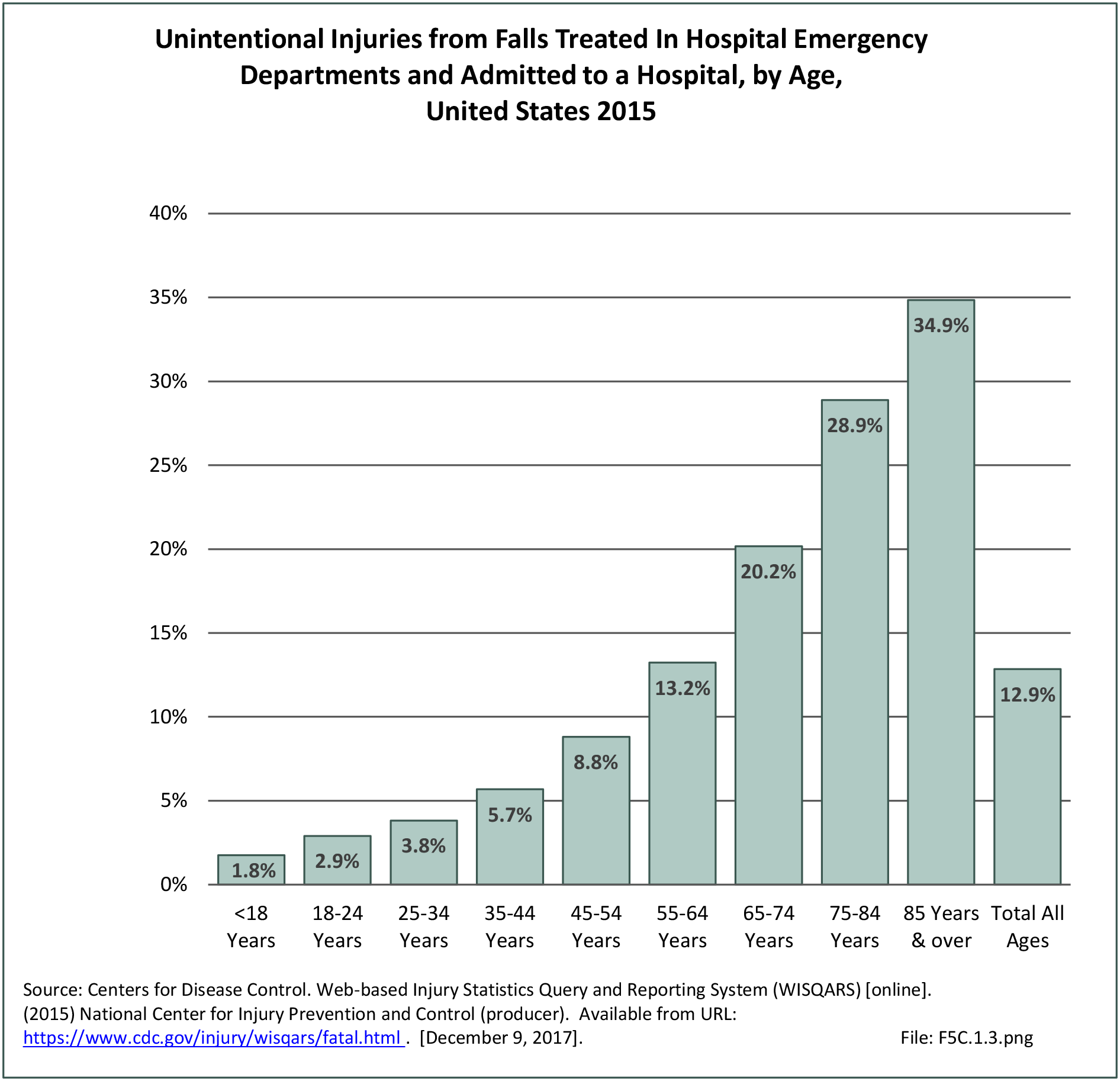
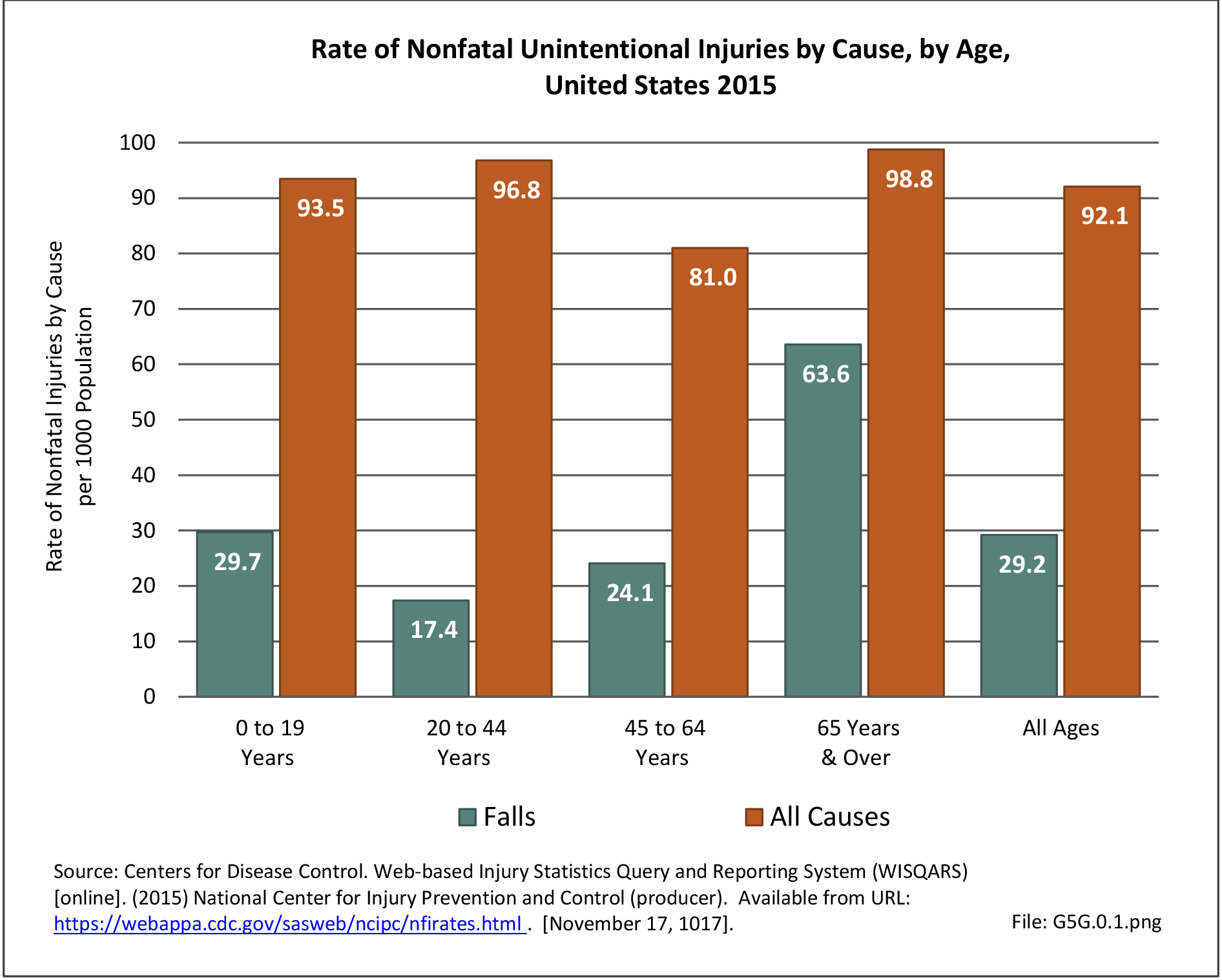
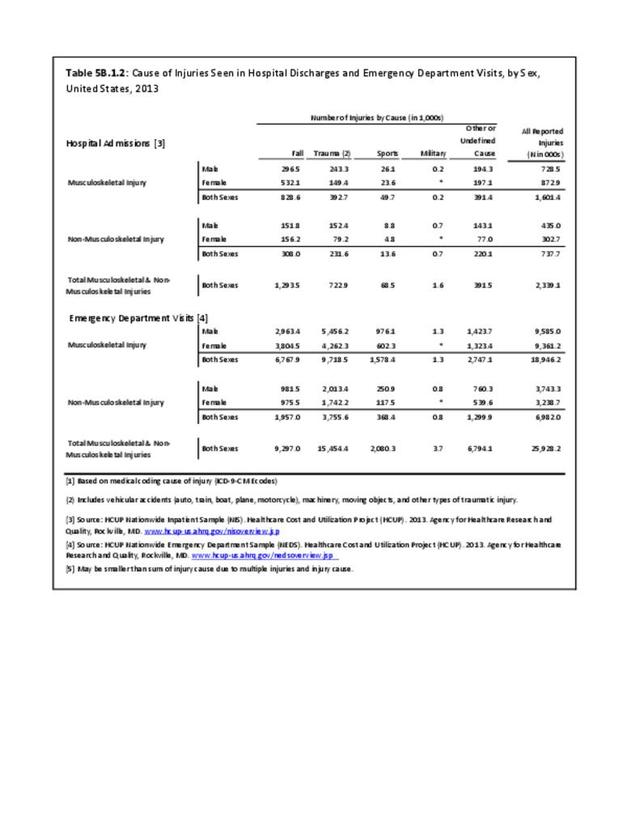
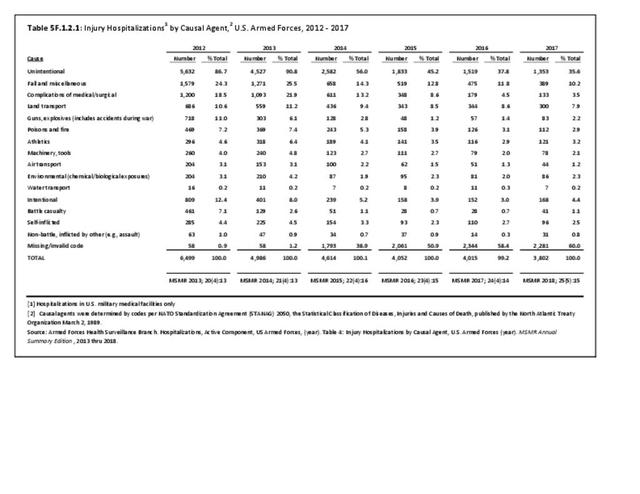
In 2012, battle injuries comprised 7% of hospitalization due to injury but fell to 1% or less in subsequent years. The overall rate of hospitalization for injuries/poisoning events has fallen over the last five years from 7.7 per 1,000 person-years in 2012 to 5.0 per 1,000 person-years in 2017. The most common cause of hospitalized injuries reported was falls. In recent years, however, the cause of more than half of hospitalizations due to injury was not identified, which makes a direct comparison challenging. (Reference Table 5F.1.2.1 PDF CSV)
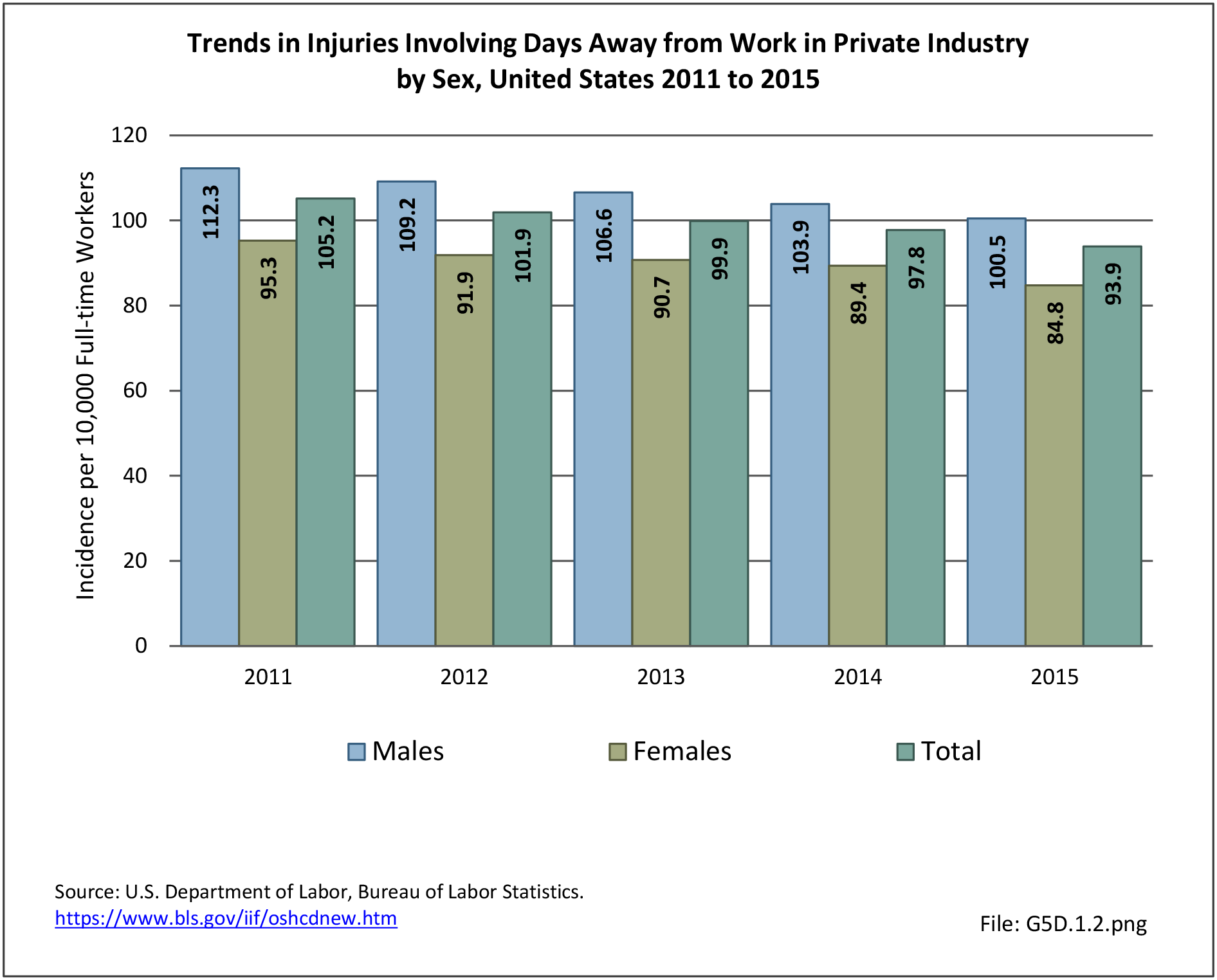
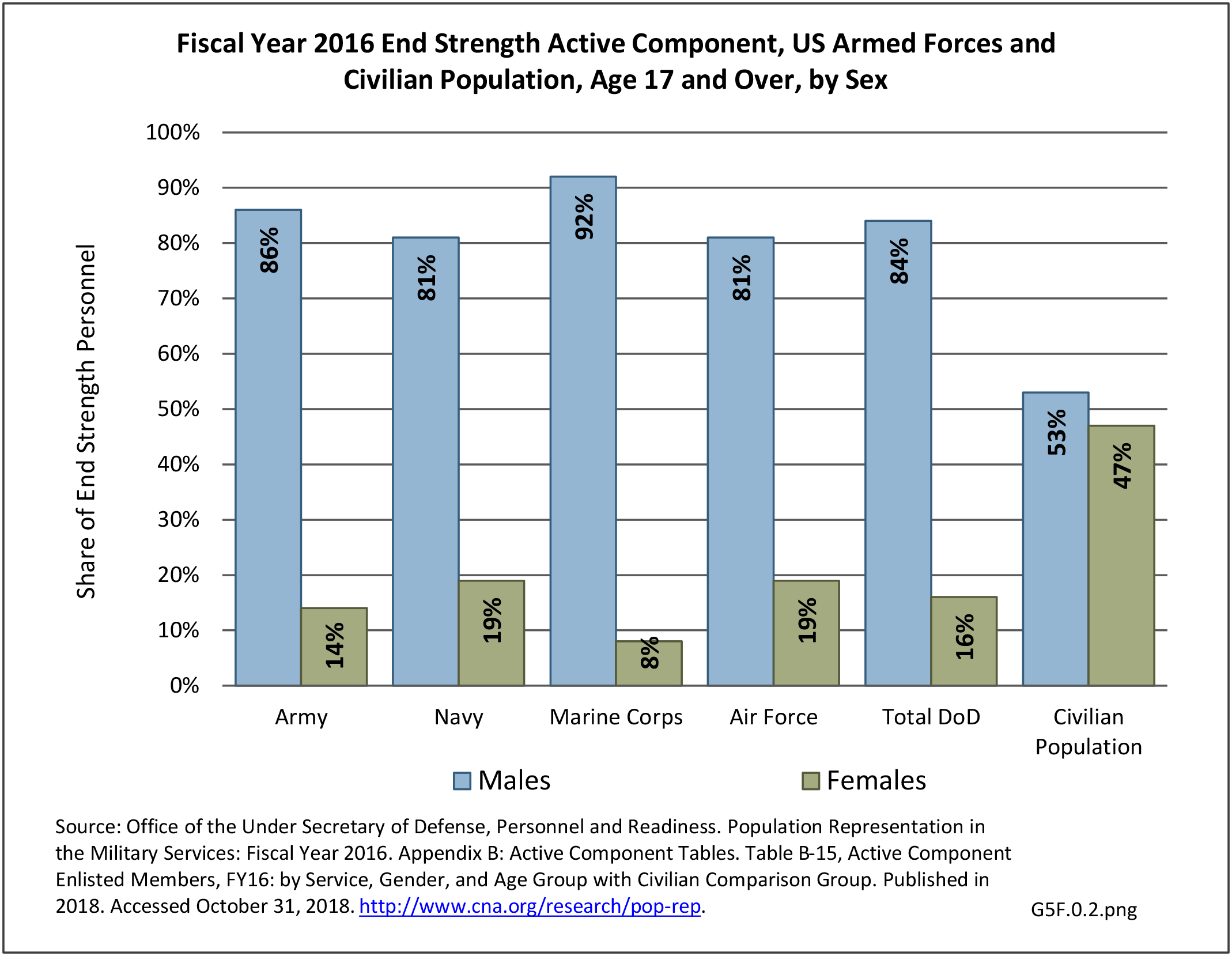
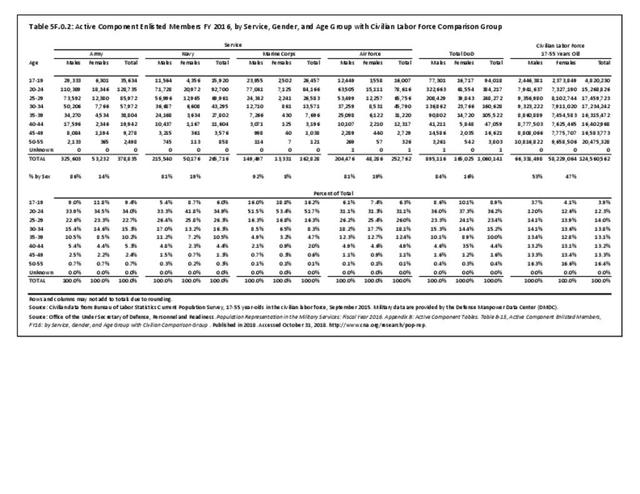
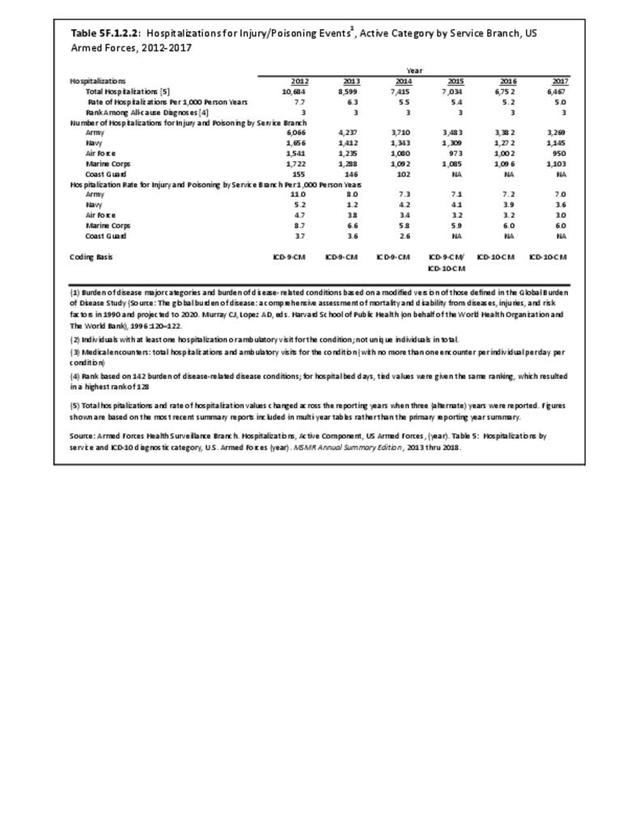
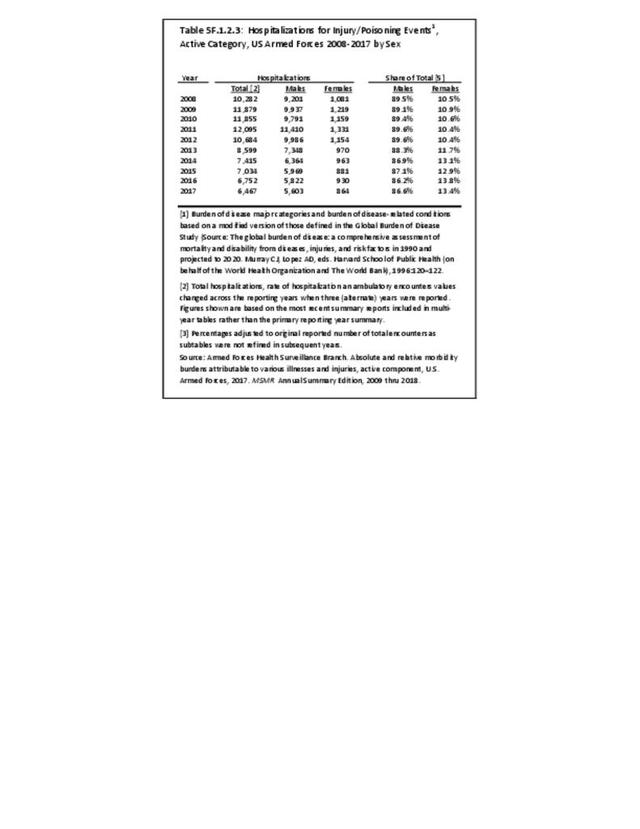
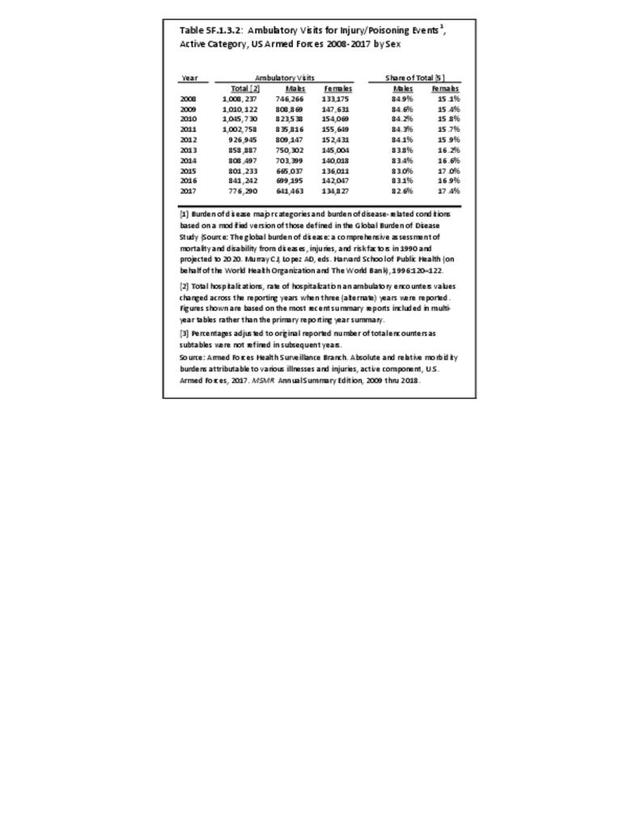
The rate of hospitalization for injuries per person-year is consistently highest in the Army and lowest in the Air Force. Based on the 2016 distribution of Armed Forces by sex (84% male; 16% female), females are slightly less likely to be hospitalized for an injury/poisoning event across all branches. (Reference Table 5F.1.2.2 PDF CSV and Table 5F.1.2.3 PDF CSV)
- 1. Cameron KL, Owens BD. The burden and management of sports-related musculoskeletal injuries and conditions within the US military. Clin Sports Med. 2014 Oct;33(4):573-89.
Edition:
- Fourth Edition